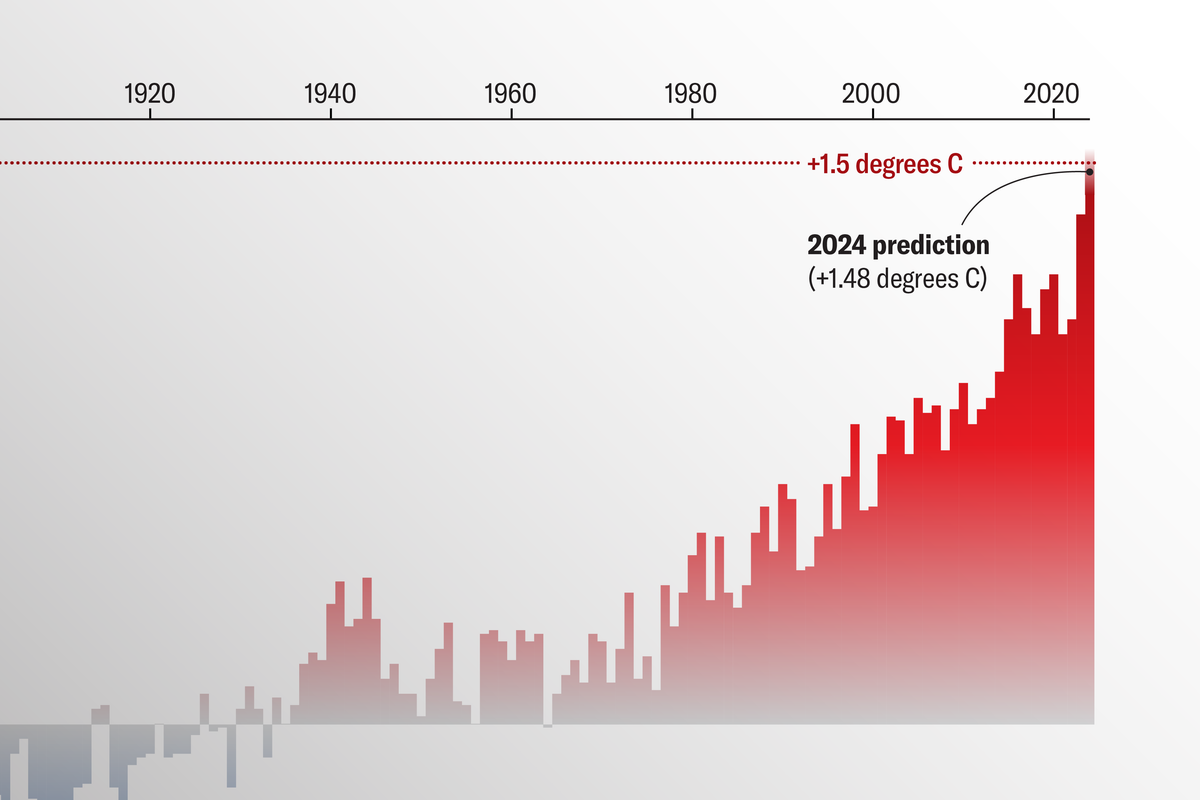
“V. vulnificus is only active at a temperature that’s above 13 degrees Celsius, and then it becomes more prevalent up until the temperature reaches 30 degrees Celsius, which is 86 Fahrenheit,” says Karen Knee, who is an associate professor and water-quality expert at American University and an open-water swimmer accustomed to ocean conditions. “I was looking at the sea surface temperature maps, and everywhere south of Cape Cod is getting into territory that’s above 20 degrees Celsius, which is when [Vibrio] really starts to become more infectious. And that’s most of the swimming waters on the East Coast.”
There’s more going on than just temperature shifts. Geoffrey Scott, the chair of environmental sciences at the University of South Carolina’s Arnold School of Public Health who leads a research consortium on oceans and climate change, says changes in water quality are whomping up Vibrio’s ability to cause severe illness. Those changes are driven by people relocating to coasts, which increases nutrient flows into the ocean via wastewater.
Vibrio used to be a late-summer hazard, but is now turning up earlier—and also later— in the year. “We’ve gone from them being mainly an issue from late July through early October, to being present April through November,” says Scott, who formerly supervised several coastal laboratories in the National Oceanic and Atmospheric Administration. “And in some cases, they have been seen overwintering in North Carolina, around the Outer Banks.”
To the problems of V. vulnificus being more virulent, in more places, for longer, you can add that more people may be exposed: first, because hot weather naturally sends more people to the beach, and second, because some of those people may not realize how vulnerable they are. “[Vulnificus] predominantly seems to impact people who have liver disease much harder than those who do not,” says Scott Roberts, an infectious-disease physician and assistant professor at the Yale School of Medicine. “And in general, being in an immunocompromised state. That could be from age, could be from chemotherapy, or if there’s some sort of underlying disease.”
Many people won’t know they are in danger. Every state with a shellfish industry participates in the National Shellfish Sanitation Program run by the Food and Drug Administration, which dictates standards for every aspect of shellfish production, including screening for contamination by Vibrio. That’s out of self-interest: Any hint of the organism’s presence can shut down a state’s shellfish economy. (In fact, since the recent deaths, the home page of the Connecticut Department of Agriculture has been topped by a highlighted banner declaring “Connecticut shellfish have never been associated with Vibrio vulnificus infections.”)
But there’s no national program that can warn swimmers or surfers of Vibrio’s presence in the ocean; no testing regime like ones that look for coastal E. coli; no system of flags like the ones that announce strong surf and rip tides. These hazards are local knowledge, shared among people who have lived alongside them.
“People down here may have a buddy who got cut on a shell or while fishing, and their finger’s a little red and swollen, and somebody will be like, ‘Don’t sleep on that. I had a buddy who waited till the next morning and he lost his hand,’” says Brett Froelich, a microbiologist and assistant professor at George Mason University in Virginia. “Other people in other locations don’t know that. They will absolutely think, ‘Well, I hope it gets better in the morning,’ and in the morning, their hand is black.”
This poses a problem: How to make the public in newly endemic areas conscious of their new risks. No one—especially not researchers at publicly funded universities—wants to be perceived as hurting coastal tourism. “We don’t want to scare people away from beaches,” Froelich says. “You don’t need to avoid [them]. You just need to be aware.”