Does it feel like we can’t catch a break? With rising COVID-19 cases, increasing cases of monkeypox and now the first case of vaccine-derived polio in the United States in nearly a decade, it feels like the hits just keep coming.
And polio was also recently detected in sewage in London, which prompted officials to encourage all residents to make sure they’re up to date with their polio shots. Additionally, Ukraine is experiencing a vaccine-derived polio outbreak.
“The big lesson, with monkeypox and polio now: What happens somewhere else in the world, it doesn’t stay there,” said Dr. Scott Roberts, the associate medical director of Infection Prevention at Yale New Haven Hospital.
So just how worried do you need to be? Below, experts shared their thoughts on this (understandably concerning) piece of news. (Hint: if you’re vaccinated against polio, you probably have nothing to worry about.)
First, don’t panic: The confirmed case does not mean the original virus is back.
“It wasn’t wild polio that was found in New York; it was vaccine-derived polio,” stressed Dr. Amesh Adalja, senior scholar at the Johns Hopkins Center for Health Security at the Bloomberg School of Public Health. “They’re related but totally different things. It’s important to remember that.”
Wild polio, which is the original virus that caused the illness many think of when they hear about the disease, has been eliminated from the United States. And remains so.
″[It] would be a major deal if we had a wild polio case. There is a major eradication program,” Adalja said. Both North and South America have been free of wild polio for a long time, “so it would be a [huge] setback if you saw a wild polio case.”
Vaccine-derived polio is different. One of the vaccines that was used to control polio around the world is called the Saven vaccine. “That is a live oral vaccine,” Adalja said, and in rare cases, the “vaccine virus can mutate and cause vaccine-derived polio if it gets into a susceptible individual,” which is what happened in New York.
“We no longer offer [the live vaccine] in the United States,” Roberts said. We offer a vaccine series in babies using an inactivated polio vaccine, meaning that there’s no risk of getting infected via the vaccine that is offered through childhood vaccination in the U.S.
The person who contracted polio in New York got it from someone who received a live vaccine in another country.
What exactly is polio?
Polio is an infectious disease that we haven’t had to worry about in the United States for decades, Roberts said.
It’s a virus “that spreads most commonly through the [gastrointestinal tract], so through fecal-oral contamination of some sort,” Roberts stated. Similar to hepatitis A, the virus spreads when people don’t wash their hands and then handle food for others.
“It’s very contagious,” he said, adding that in the days before widespread vaccination, if someone brought it into a household, there was a high likelihood that everyone in the house would get infected.

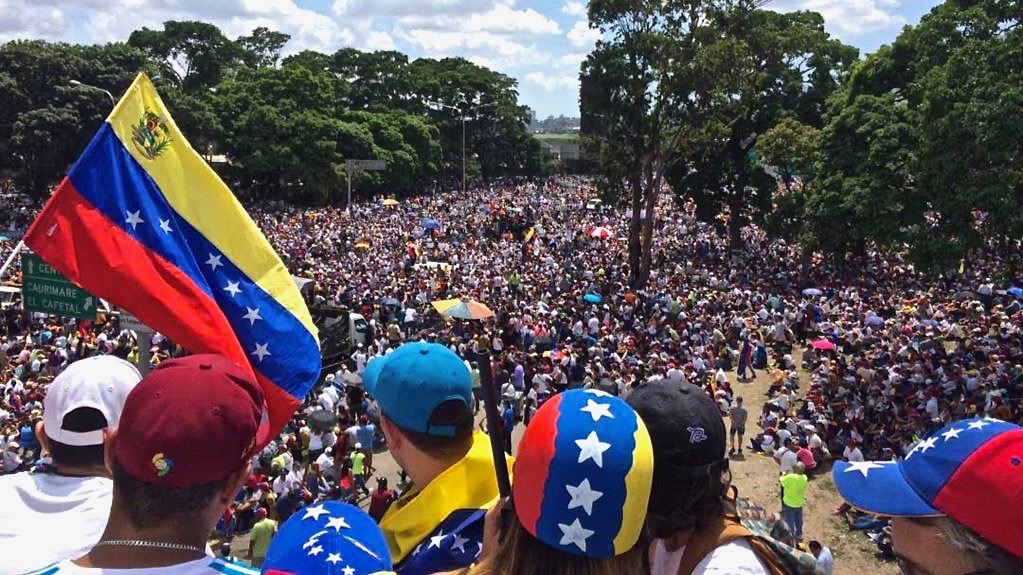
Catherine Falls Commercial via Getty Images
What are the symptoms of polio?
According to Roberts, most people who contract polio will never know it. About three-quarters of the people who get infected have no symptoms at all. And roughly one-quarter of infected people will have a flu-like illness that goes away in a few days.
“The reason polio is concerning and everybody used to be really scared of [it] is that a small subset of people, about 1 in 200, can get paralysis that is irreversible,” he said.
Good news: People who are vaccinated against polio are largely not at risk for developing the virus.
If you’re vaccinated against polio, you likely have nothing to worry about.
“The threat to the general public is very low — especially since the vast majority of the general public is vaccinated,” Roberts said.
According to Adalja, over 90% of the U.S. population is vaccinated against polio.
But unvaccinated people are at risk.
“There is a risk if there are enclaves of unvaccinated individuals,” Adalja said. “So if you’re in a place where there are unvaccinated people, these vaccine-derived strains can spread.”
It’s important for people to stay up to date with their vaccinations, he added, noting that vaccines have faltered after the COVID-19 pandemic. Particularly, childhood immunizations have fallen.
Unvaccinated children and adults would both be at risk if vaccine-derived polio spreads beyond the case in New York.
People with certain medical conditions could be at risk, too.
Some people who are undergoing specific medical treatments, such as cancer patients who are on therapy that blocks their antibody response to vaccination, or people who have had stem cell transplants, may need to talk to their doctor about additional precautions.
You have to revaccinate these vulnerable groups after treatments sometimes because the immune system is kind of starting new, Roberts said.
The Centers for Disease Control and Prevention’s current guidance for high-risk individuals states that “higher-risk adults who have had three or more doses of polio vaccine in the past may get a lifetime booster.”
If you’re at high risk, it’s worth reaching out to your doctor for additional guidance ― not just because of this case, but because overall it’s a good idea to make sure your vaccinations are all OK.