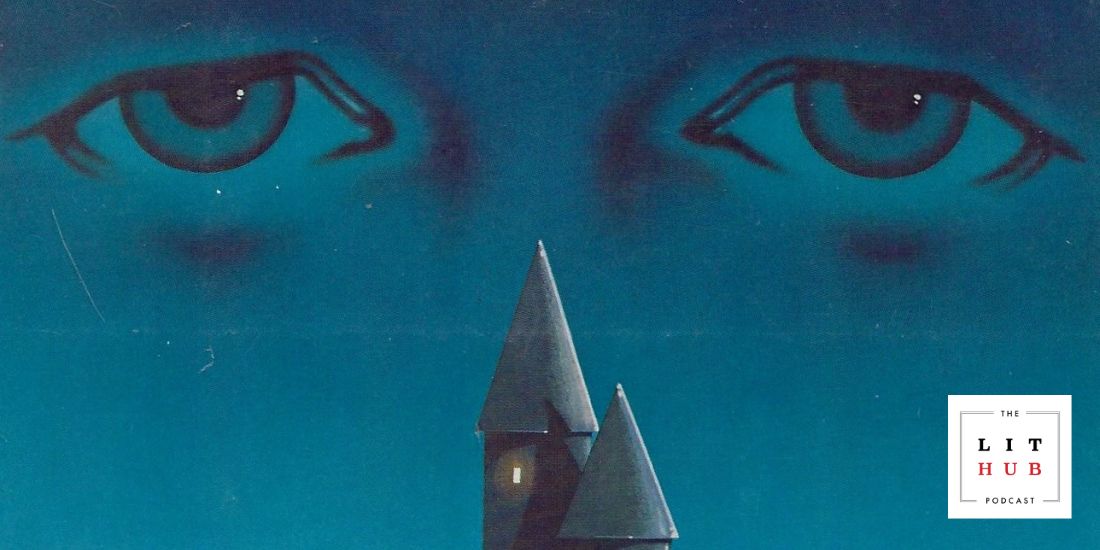
As I heard the sci-fi clangs and bellows of the MRI scanner, all that rang through my mind was the near-familiarity of this experience. As a neuro-oncologist, I have often listened to my patients’ experiences in MRI scanners, from the loud noises to the claustrophobic abyss, and seen their anxiety that preceded the results.
Though I have had MRIs before, this time felt different, possibly because of the proximity to my own neurological awareness and because of the intimacy of having this scan performed in my own hospital’s facility.
When the phone rang the next day and my otolaryngologist said the words, “You have an acoustic neuroma,” I surprisingly phewed a sigh of relief. Because my aunt, grandmother, and great-aunt all died of what was likely glioblastoma, I have cautiously expected the most-feared of malignant brain tumors and anticipated that someday I would hear those fateful words. In actuality, all I could think was that as long as it wasn’t a glioblastoma, I would readily accept any other diagnosis.
After the diagnosis, the whiteboard in my mind was a flurry with pro/con list-making. I distilled my experiences with other patients and ultimately decided to pursue surgery at the outset. At the same time, the chasm in my physician-patient body opened ― how would I cope from brain tumor surgery and would I set a good example for my patients by maintaining resilience through the process?
On a crisp October day, I entered the hospital, ready for the 7.5-hour surgery, knowing that I would lose hearing on my right side, cautious about preservation of my facial function, but most of all, eager to have the tumor out. When I awoke and discovered my facial function had been largely preserved, I was relieved: I’ve always valued my smile. I heard the typical post-operative whooshing tinnitus and vomited four times immediately after receiving my first intravenous steroid dose. In the hundreds of patients I’ve ordered dexamethasone for, I’d never heard of anyone vomiting, despite this apparently well-known idiosyncratic effect.
Unfortunately, those weren’t the last of the post-operative complications. Salty spinal fluid started dripping out of my nose and down my throat, and I spent 12 days in the hospital to address this problem. One of my attendings during neurology residency often said that complex hospitalized patients needed to go on “all the rides.” The same could be said of me, cast in the role of the patient in a hospital drama where I was usually the one standing at the bedside. Though these days in bed were by no means pleasant, the journey awakened my inner physician, allowing me to diagnose each new setback and formulate a plan of action.
After I was hospitalized for 12 days and lost 11 pounds during that time, I realized just how feeble one can be after spending so long in bed ― and with so many days of nausea and lack of sleep. Flashbacks to my patients’ requests to see the physical therapist more than twice a week encircled me. I, too, longed for a better position to eat in bed. For the first time in my medical career, I truly internalized that patients often measure their care not in billable procedures and medical decision-making but in predictable simplicities.
I chose the next days’ meals each afternoon, timed my teams’ morning rounds within a 5-minute window, and squinted up at the clock each evening at 11 p.m. just as I was awoken by the nurse to take my evening vital signs. Even more, I processed my experience in the context of my patients, an “ah ha” bell ringing daily with the newly recognized truths they told me as I sat across from them in clinic.
I was discharged on a blindingly sunny November day, hoping for a bumpless ride home with my head wrap precariously positioned against the back seat. After settling into my new routine, all that preoccupied my mind was returning to my lab and clinic, taking my own diagnosis out of the limelight and lowering this whole journey to background noise. What I didn’t expect in the days and weeks after my surgery was how much this experience would inform my practice. As a junior attending, I routinely convey brain tumor diagnoses or sit across from my patients as they tell me all they want to do is go home, all the while helping them mentally cope with their cancer.
Gradually, I began to glimpse the hospital environment from the vantage point of a physician-patient, zooming out from the day-to-day bustle on the wards and magnifying the alterations that this journey has had on my professional encounters.

Recently, a patient was fearful of undergoing brain tumor surgery, afraid of what she would feel like afterward and apprehensive of surgical site pain. Without a moment wasted, I chimed in, “I went through this same surgery, and here I am in front of you, doing just fine.” I felt a sigh of relief from my patient, as though our therapeutic alliance had morphed into a familial connection.
I began to ponder when to share ― and consider not sharing ― details of my journey. For example, I recognize that my diagnosis of a benign brain tumor may pale in comparison to the incurable malignancies growing within many of my patients’ brains. Even worse, my surgical cure may be at odds with their experiences and may be counterproductive to an empathic therapeutic connection. Likewise, I am careful not to shift the focus of my patient encounters to me: Office visits are meant to address their concerns, not to coerce them into a provider role to facilitate my own recovery.
Even when not sharing my own experience, I have found that patients’ stories can be quite triggering. Recently, a patient told me that after she returned home from her own brain tumor surgery, she fainted in the tub after showering for the first time. She said the heat and flowing water were all too much for her. As I heard her story, I felt immediate resonance. When I stumbled into the shower awkwardly for the first time after surgery, holding onto the curtain rod to step in and the towel bar to steady myself amid the rush of warm water over my body, I felt like a clumsy skeleton. The sensation felt somewhat allodynic but also refreshing, as if the water was cleansing off nearly two weeks of hospital gunk.
With these experiences, I have learned that sharing my story is not without risks ― of over-sharing, of my own vulnerabilities coming out, and even of triggering encounters, for myself and my patients. I even wondered whether these triggering experiences would alienate me from my patients, forcing me to bury my own medical record. But having been on the receiving end of a difficult diagnosis, of tiptoeing into an MRI machine, and of having a tumor tweezed out of my brain, I know that shielding myself from my patients backfires, preventing ignition of a therapeutic “on” switch. Personal stories of my physicians and friends living with single-sided deafness or hearing about coping strategies for dizziness were the fuel in my recovery engine.
Though I don’t have a precise algorithm for when to share my own experience as a patient in neuro-oncology, I generally rely on cues from my patients as a guide. Some patients may be afraid of undergoing surgery, not understanding what a surgical scar might feel or look like in the weeks after surgery. Some patients may worry about post-operative pain or wonder what it’s like to lose hearing on one side. In these instances, I find that my experience can help them prepare for surgery, taking the edge off the anxiety of proceeding with a major surgery. I emphasize that undergoing brain tumor resection, recovering from surgery, and learning how to return to life is difficult ― but possible. I talk about the problems I have faced with unilateral deafness, or how to regain balance, or to make sure to eat as well as possible in the hospital. I emphasize physical therapy for the wondrous benefit it had on my return to work and life.
So far, I have shared my experience with about half a dozen patients in whom I sensed fear and apprehension about brain tumor surgery or their post-operative recovery. I have leveraged my own experience not to convince patients of my clinical recommendations, but to illuminate one possible path of recovery. In all of these situations, I feel that this sharing has helped ― rather than harmed ― the relationship with my patients.
Though not all physicians commiserate with their patients’ journeys, we all bring our personal lives to our patients ― whether we admit it or not. What I find most useful when looking through the lens of this past year is that thoughtful sharing can humanize us in the eyes of our patients. Our patients look to us not just for our professional opinion but often our personal opinion on the right direction of care. And sharing direct medical experience as a patient or loved one can ring true for them, validating these opinions and comforting our patients during isolating periods of decision-making.
As a physician, this process has taught me that our experiences can be relevant to our patients and that appropriate sharing is a powerful means to better connect with our patients. Having been strapped into the metal mask atop the MRI gurney before my surgery and waking up with a C-shaped line of sutures concealed behind my ear after surgery, I now consider this experience perhaps the most useful tool that I can bring to my clinic.
Dr. Evan Noch is assistant professor of neurology within the Division of Neuro-oncology at Weill Cornell Medicine-New York-Presbyterian Hospital. Dr. Noch earned his M.D. and Ph.D. degrees from Temple University before completing his residency in neurology at Weill Cornell Medicine and fellowship in neuro-oncology at Memorial Sloan Kettering Cancer Center. In addition to his clinical pursuits, he conducts basic and translational research on metabolism in malignant brain tumors and leads a company developing mobile technologies for clinical stroke detection.
Do you have a compelling personal story you’d like to see published on HuffPost? Find out what we’re looking for here and send us a pitch.