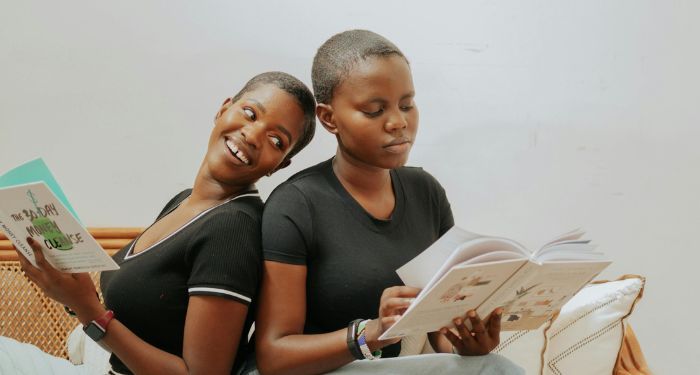
Volunteers have been exposed to the coronavirus that causes covid-19 as part of a scientific study
koto_feja/GETTY
Deliberately exposing people to the coronavirus behind covid-19 in a so-called challenge study has helped us understand why some people seem to be immune to catching the infection.
As part of the first such covid-19 study, carried out in 2021, a group of international researchers looked at 16 people with no known health conditions who had neither tested positive for the SARS-CoV-2 virus nor been vaccinated against it.
The original variant of SARS-CoV-2 was sprayed up their noses. Nasal and blood samples were taken before this exposure and then six to seven times over the 28 days after. They also had SARS-CoV-2 tests twice a day.
The participants fell into three groups, says team member Sarah Teichmann at Cambridge Stem Cell Institute in the UK. In one group, six people tested positive in both of their daily tests for more than two days, while also having symptoms. In another, three participants tested positive in one of their twice-a-day-tests, but not the other, for no more than two days, without symptoms. In the final group, seven people consistently tested negative for the coronavirus.
In total, the researchers looked at more than 600,000 blood and nasal cells across all the individuals.
They found that in the second and third groups, the participants produced interferon – a substance that helps the immune system fight infections – in their blood before it was produced in their nasopharynx, the upper part of the nose behind the throat where the nasal samples were taken from. The interferon response, when it did occur in the nasopharynx, was actually higher in the noses of those in the second group than the third, says Teichmann.
These groups also didn’t have active infections within their T-cells and macrophages, which are both types of immune cell, says team member Marko Nikolic at University College London.
The results suggest that high levels of activity of an immune system gene called HLA-DQA2 before SARS-CoV-2 exposure helped prevent a sustained infection.
Nikolic hopes the findings will improve understanding around the cell responses associated with covid-19 protection, which could assist vaccine and treatment development.
“This study serves as a unique resource of previously uninfected SARS-CoV-2 participants due to its carefully controlled design and real understanding of ‘time zero’ for when the infection took place in order to measure the immune responses that follow,” says José Ordovas-Montanes at Harvard Stem Cell Institute in Massachusetts.
However, most people have now been exposed to “a veritable mosaic of SARS-CoV-2 variants”, rather than just the ancestral variant used in this study. The results may therefore not reflect cell responses outside of a trial setting, he says.
Topics: