Researchers identified receptors in the vagus nerves of mice that help control inflammation, which could improve treatments for conditions such as rheumatoid arthritis where the pathway may malfunction
Health
18 January 2023
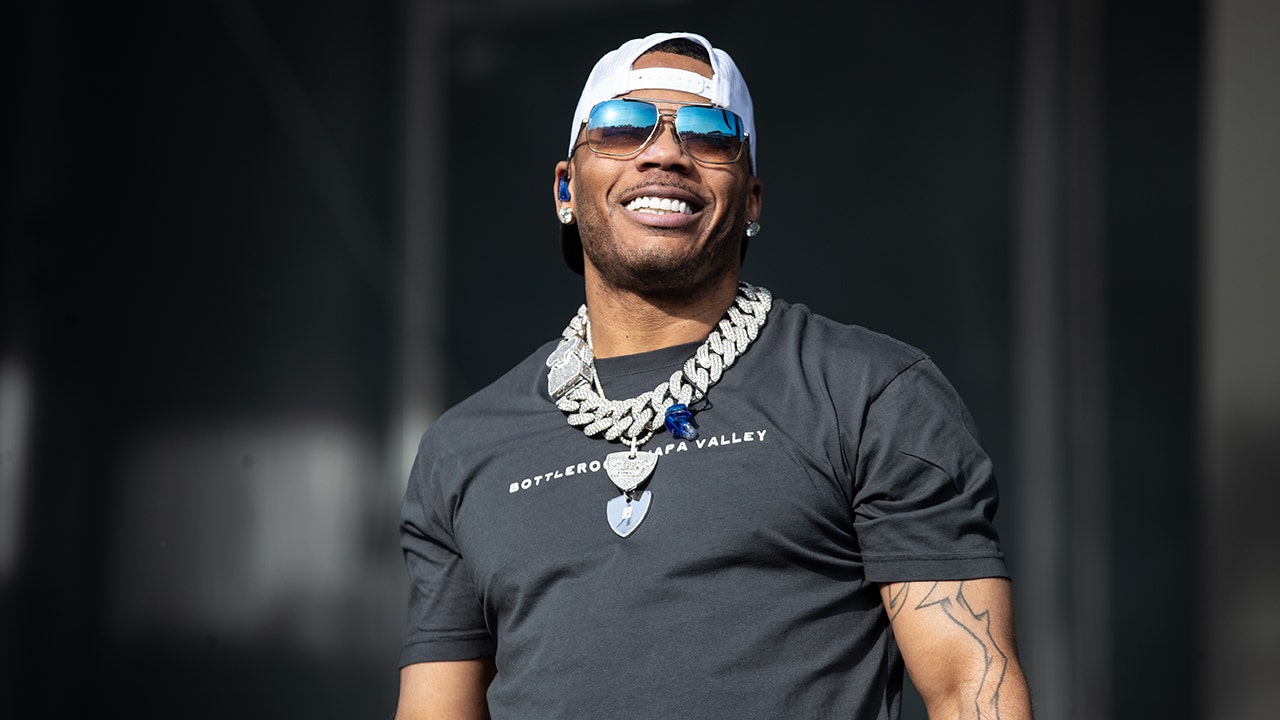
Conditions such as arthritis could be treated by targeting receptors in the vagus nerve that control inflammation Kobus Louw/Getty Images
Specific receptors in the vagus nerve help detect and control inflammation in mice. If the same is true for humans, these receptors could be the target of future therapies for inflammatory conditions such as rheumatoid arthritis and multiple sclerosis.
“Inflammation is our body’s response to injury and infections,” says Kevin Tracey at the Feinstein Institutes for Medical Research in New York. Left unchecked, this reflex can turn against us as excessive inflammation damages cells and contributes to chronic disease. “When it’s controlled, it drives healing and recovery,” he says.
It’s well known that the brain sends signals for controlling inflammation through the vagus nerve, but it was previously unclear how the brain knows when to turn off inflammation. “We didn’t know what activated the brakes,” says Tracey.
To determine this, he and his colleagues studied eight mice, half of which had been genetically engineered to lack a specific type of receptor in the vagus nerve that is sensitive to some inflammatory molecules.
Proteins called cytokines are the main drivers of inflammation, so the researchers injected the mice with a type of cytokine known to induce changes in body temperature. They found that the genetically engineered mice maintained their temperature while the others developed hypothermia, suggesting the vagus nerve receptors are necessary for the body to detect inflammation.
Next, the team injected a toxic molecule into a separate group of 19 mice to induce a cytokine storm, which is when an overproduction of cytokines causes life-threatening inflammation. They activated the vagus nerve receptors in 10 of these mice using optogenetics, a technique to turn cells on and off using light. The mice produced half as many cytokines on average as those that didn’t have these receptors activated and saw significantly reduced inflammatory damage.
Taken together, these findings indicate that these specific receptors in the vagus nerve not only detect inflammation but keep it in check by signalling to the brain when inflammatory responses need to be turned off.
Tracey says these findings are important for two reasons. The first is that they provide “a new way to think about how the brain and nervous system interact with the immune system to control the outcomes of infection and injury”. Second, he says these receptors could guide the development of new therapies for people with chronic conditions characterised by excessive inflammation.
For example, clinical trials have shown that stimulating the vagus nerve with electrical pulses can reduce symptoms and even slow the progression of diseases like epilepsy, inflammatory bowel disease and multiple sclerosis. These findings raise the possibility of developing ultra-selective vagus nerve stimulators that act only on receptors known to control inflammation, which could improve treatment outcomes, says Tracey.
Sign up to our free Health Check newsletter for a round-up of all the health and fitness news you need to know, every Saturday
More on these topics: