This podcast was produced for the Lung Cancer Initiative at Johnson & Johnson by Scientific American Custom Media, a division separate from the magazine’s board of editors.
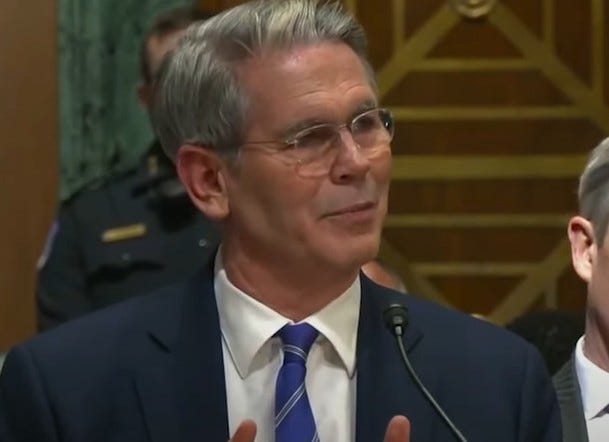
Avrum Spira, MD, MSC, Global Head of the Lung Cancer Initiative (LCI) at Johnson & Johnson, shares his perspectives as a pulmonary and critical care physician and vision for transforming this deadly disease. He discusses how the LCI is taking an interventional approach to target the root cause of the disease, better understand the needs of patients and physicians and innovate with less invasive and more precise treatment options for early-stage lung cancer.
Transcript:
Megan Hall: Any cancer diagnosis is devastating, but patients with lung cancer face an especially daunting journey. Lung cancer is the leading cause of cancer deaths in the world. It’s difficult to detect in its early stages and hard to treat once it’s finally discovered.
But there’s hope on the horizon.
Dr. Avrum Spira is leading a multidisciplinary team that’s taking a convergent approach to target the root cause of the disease and detect lung cancer before it develops to help improve patient outcomes.
It’s all part of his efforts as Global Head of the Lung Cancer Initiative at Johnson & Johnson.
Scientific American Custom Media recently sat down with Dr. Spira to learn more about his work and the future of lung cancer treatment.
Hall: Dr. Avi Spira learned about the devastating effects of lung cancer early in his career.
Avi Spira: I was a medical resident at that time, and all of a sudden, I got a call one weekend.
Hall: It was about his aunt.
Spira: She was full of life. Always, since I’ve known her from a young age. And she had lived a very healthy life, never smoked, exercised, ate well.
Hall: But, she had fluid around her lungs
Spira: And it turned out within a few days, they diagnosed her as having stage four lung cancer. And her prognosis was, she would only live a few months.
Hall: While she fought valiantly against the disease, she died within a year of her diagnosis
Spira: Watching her take her last breath was incredibly traumatic. But also, I realized at that point in my career that I wanted to do something to change the trajectory of this disease.
Hall: Avi’s aunt was a case of a non-smoker getting lung cancer
Spira: Lung cancer is the most lethal cancer because it’s almost always diagnosed at an advanced stage.
Hall: It’s easy to not know you have lung cancer, because of the way it develops.
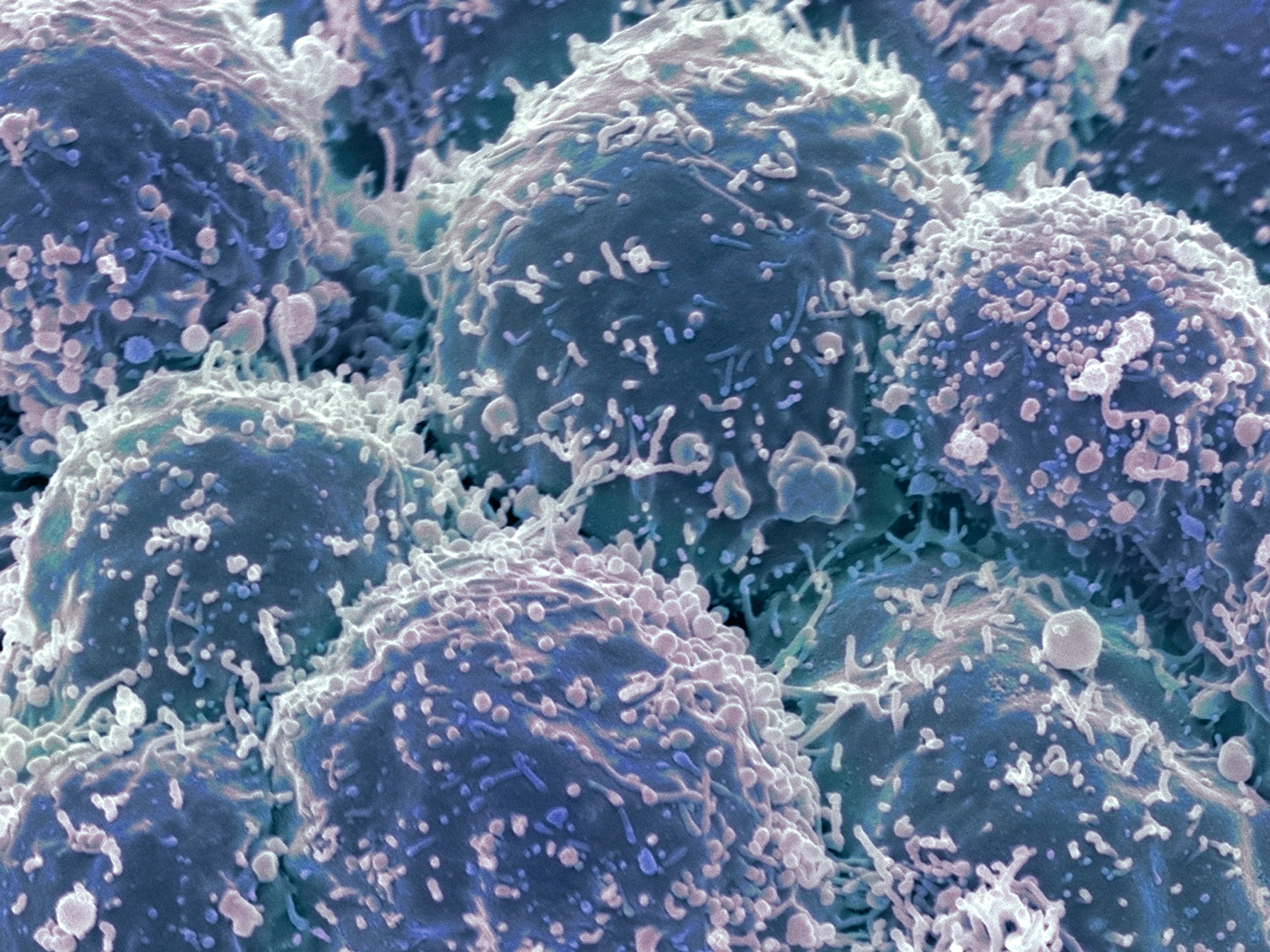
Spira: It starts insidiously as a little, small group of cells deep within your lung tissue, doesn’t impair your breathing, you don’t have chest pain, you’re not coughing up blood, and it grows silently over months, and potentially years. And by the time you start feeling it, it’s too late.
Hall: As Avi moved forward with his career he did so with a focus on the early detection of lung cancer.
Spira: As an academic, I spent 15 years making some amazing discoveries in the lung cancer space about diagnosing lung cancer earlier, but it was so hard to translate those discoveries into patient benefit, very hard to do as an academic.
Hall: Avi wasn’t satisfied with those discoveries. He wanted to see them used in the real world to help patients — right away.
Spira: I became a serial entrepreneur. And I started three companies, one of which took one of my early detection tests for lung cancer, and successfully commercialized it.
It took us over a decade to go from the discovery in 2007 to seeing it actually in the clinic helping patients.
Hall: That’s why, while he was working as a consultant for Johnson & Johnson, he saw an incredible opportunity. The company was looking for a way to use the full breadth and depth of its resources to transform the way we prevent, detect, and treat a specific disease.
Spira: We made a very strong case to leadership at Johnson & Johnson that there’s no disease that’s a bigger unmet need right now worldwide than lung cancer, in terms of a holistic cross-sector solution.
Hall: So you were kind of whispering in their ear and saying, Hey, do lung cancer first?
Spira: I think I was more than whispering. I may have been yelling a little bit. At the time, as a physician on the front lines, I was seeing day in and day out what this disease was doing to my patients, to their families, to society, to the world — the cost of the disease. And I felt this was a disease, more than any other, in need of a new approach — transformative innovation. I couldn’t imagine any company in the world that could do it the way J&J could, given that they had medical devices and pharmaceuticals under the same umbrella.
Hall: Leadership listened. With support from Dr. Bill Hait, who was Global Head of External Innovation at the time, the Lung Cancer Initiative at Johnson & Johnson was formed in 2018 and Avi became the Global Head. Since then, he’s assembled a diverse team from inside and outside the company.
Spira: I call it the dream team that we’ve been able to put together. And that’s because I think it’s relatively unique to have deep, deep expertise in medical devices alongside very deep expertise in pharmaceuticals, all under one roof. So what that allows us to do is really put together a multidisciplinary group of scientists, clinicians, all the support staff, that one would need to go out and create unique solutions that were previously unimagined for this disease.
Hall: In the four years since the Lung Cancer Initiative was formed, Avi’s team has been working to address the two biggest unmet needs along the patient journey. Think about a robotic bronchoscope that could make it easier to tell if a growth or spot on someone’s lung is cancerous or not.
Spira: It’s an endoscope that goes through your mouth or nose that’s robotically controlled and can snake its way out in a relatively non-invasive way, all the way out to previously unreachable parts of your lung.
Hall: Once this bronchoscope reaches that distant part of the lung, it can take a small sample of the growth to test for cancer cells. But there’s more to the vision of the Lung Cancer Initiative at Johnson & Johnson. Dr. Spira, can you share what could happen in the future to address other unmet needs?
Spira: We are excited to use this robotic bronchoscope to not only go out and diagnose lung cancer earlier, which was that first unmet need, but in that procedure also to treat the lung cancer by injecting a drug or energy directly into it through the bronchoscope. And having a less invasive, more precise way of treating and more effectively treating that disease
Hall: It’s very exciting to hear that one day in the future you may be able to treat within a tumor, known as intratumoral therapy, and we hope Dr. Spira will come back again to tell us about additional progress made. The Lung Cancer Initiative is also working with a global consortium on something called a “pre-cancer atlas,” which is exciting in terms of looking to go deeper in understanding the disease. Can you tell us about this?
Spira: What a precancer Atlas is, is — think about all of the cellular and molecular changes that occur as a normal cell in your lung becomes pre-cancer and eventually becomes a full-blown invasive cancer. So it’s a map of all of those changes.
Hall: Avi’s team hopes to use that map in the future to identify the earliest signs of lung cancer development before it becomes a clinical problem.
Spira: And the analog here is cardiovascular disease. You know, in the last 30/40 years, cardiologists no longer wait for someone to get a full-blown heart attack to start treating the patient. They treat the patient years and decades before they get disease. And they’re able to do that because they gain the fundamental root-cause understanding of what drives the earliest part of their disease.
Hall: Avi is hoping to find ways to identify that someone is on their way to developing lung cancer.
Spira: If we had that map of the molecular changes of a pre-cancer to a cancer, we could develop ways of finding people that are harboring these precancerous lesions, and then blocking them from ever getting an invasive disease.
Hall: Would these future developments have prevented his aunt from dying? Avi says maybe not in the short term. She was a non-smoker, so she probably wouldn’t have gotten a screening for lung cancer.
Spira: But I do think in that longer-range future a non-invasive blood test or a nasal swab, or some sort of breath test could be done every year at your annual family doctor visit. My aunt could have had one of those tests when she was in her late 30s, early 40s, and then had some sort of treatment that would have prevented her from getting the disease in the first place, or at least then get followed very closely.
Hall: Thanks to the work of the Lung Cancer Initiative, Avi believes a future like that is possible. A future that includes earlier diagnosis and treatment all in one procedure…and a transformation of the lung cancer care paradigm that will help impact millions of people around the world.
Hall: Dr. Avrum Spira is the Global Head of the Lung Cancer Initiative at Johnson & Johnson. He is also an attending physician in the Medical Intensive Care Unit at Boston University Medical Center and a Professor of Medicine, Bioinformatics and Pathology at Boston University. The Lung Cancer Initiative was formed in 2018 to unleash the full potential of science and technology to change the trajectory of this complex disease.
This podcast was produced by Scientific American Custom Media and made possible through the support of the Lung Cancer Initiative at Johnson & Johnson.
Learn more about how Johnson & Johnson is taking a multi-disciplinary approach to tackle lung cancer.








































![Transforming the Trajectory of Lung Cancer [Sponsored] Transforming the Trajectory of Lung Cancer [Sponsored]](https://static.scientificamerican.com/sciam/cache/file/FC422525-0328-4B23-A9B455789B364A12.jpg)