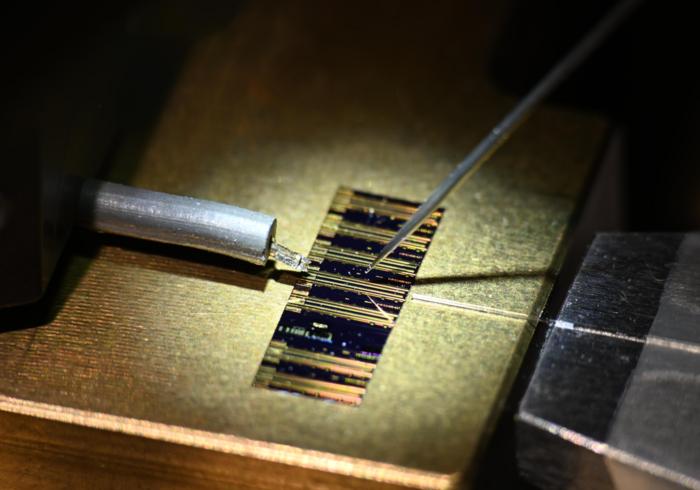
Over the course of several months, each fascicle would grow into the muscle, resupplying it with nerve signals. By placing an electrode into the little muscle-nerve bundle, scientists could record in real time which nerve signals were coming from each fascicle. “Then, instead of trying to record tiny nerve signals, you get to record these hugely amplified muscle signals,” Cederna says. “That little piece of muscle acts as a bio-amplifier, and now you can hear what a nerve is saying.”
Ortiz-Catalan’s group learned this technique from Cederna and decided to expand it. In addition to using muscle grafts from other parts of the body (in their case, the leg), they decided to reroute some of the dissected nerve fascicles to existing muscles in the arm. This technique of transferring nerves to existing muscles, known as “targeted muscle reinnervation,” had been used before to help with prosthetic control. Combining both strategies, Ortiz-Catalan says, gave them “the best of both worlds”—more electrical nerve signals that could be translated into different movements.
To send all this nerve information to an actual prosthesis, Ortiz-Catalan and the team connected the implanted electrodes to a titanium implant drilled into the patient’s humerus bone in the upper arm. The implant facilitated two-way communication between electrodes in the body and the external prosthesis. This was no small feat: Starting from the drilling of the implant, the entire process took over six months, including a 12-hour surgery to reroute all the nerves.
Once all was in place, the scientists could monitor how their implanted electrode system communicated with the prosthesis. First, they tracked the electrical signals from each implanted electrode. While fuzzy at first, the signals became much stronger. According to Jan Zbinden, a PhD student in Ortiz-Catalan’s lab and study coauthor, this meant that the nerve fascicles were successfully integrating into their respective muscles and supplying them with adequate signals.
By using machine learning algorithms, the scientists could map these signals to specific movements the patient was trying to make—opening his hand, for instance, or lifting the index finger. Each movement could then be programmed into the prosthetic, so that each type of electrical signal would cause the corresponding movement in the artificial limb.
Around four months after the surgery, the patient was able to complete basic movements like flexing his wrist and opening his hand, as well as moving each finger. After a little over a year, the scientists noticed that the patient could intuitively move his prosthesis. This meant that rather than having to think of each movement as a multistep procedure, he could simply just think of the movement, try to execute it, and it would happen. “If you have to think, ‘biceps, triceps—open. Close hand,’ that creates cognitive load,” Zbinden says. “It’s a bit more difficult than to think, ‘Oh, now I want to move my thumb.”
Today, over two years after the procedure, Zbinden says that the patient is still using the prosthetic: “Currently, he can open and close the hand, rotate the hand, flex and extend the elbow, all by thinking about it.”
This prosthetic platform, in which the patient can move all five fingers independently, is “very exciting and presents something very new,” says Oskar Aszmann, a plastic surgeon at the Medical University of Vienna in Austria who was unaffiliated with the study. He is curious to see if this platform can one day become wireless—something that is difficult due to the sheer amount of information transmitted back and forth through the electrodes and prosthesis. Both he and Cederna note, though, that the findings need to be replicated in other patients.
Ortiz-Catalan and Zbinden agree. They’re continuing to refine the prosthetic platform and are interested in adding sensory feedback. In the meantime, though, they look forward to participating in the next Cybathlon with their patient. “He’s a guy who does stuff with his hands,” Ortiz-Catalan says. “He has a really physical job, works in a workshop, and seeing him use the device in his daily life—seeing that the connections work and how the function increases—that’s one of the most rewarding things that we have.”