To go through life in a fat body means you are less likely to be hired for a job and will be paid less than non-fat people. The effects of weight discrimination—which can include poorer medical treatment, loneliness, psychological distress, and increased stress—may actually be cutting short the lives of fat people.
Deciding whether to take the drugs becomes a “devil’s choice,” says Osborn. “Assert that I have the right to be as I am right now—or exchange that right for significantly more rights and privileges in the culture.” The fat acceptance movement instead pushes for fat people to be afforded the same rights as everybody else, regardless of size.
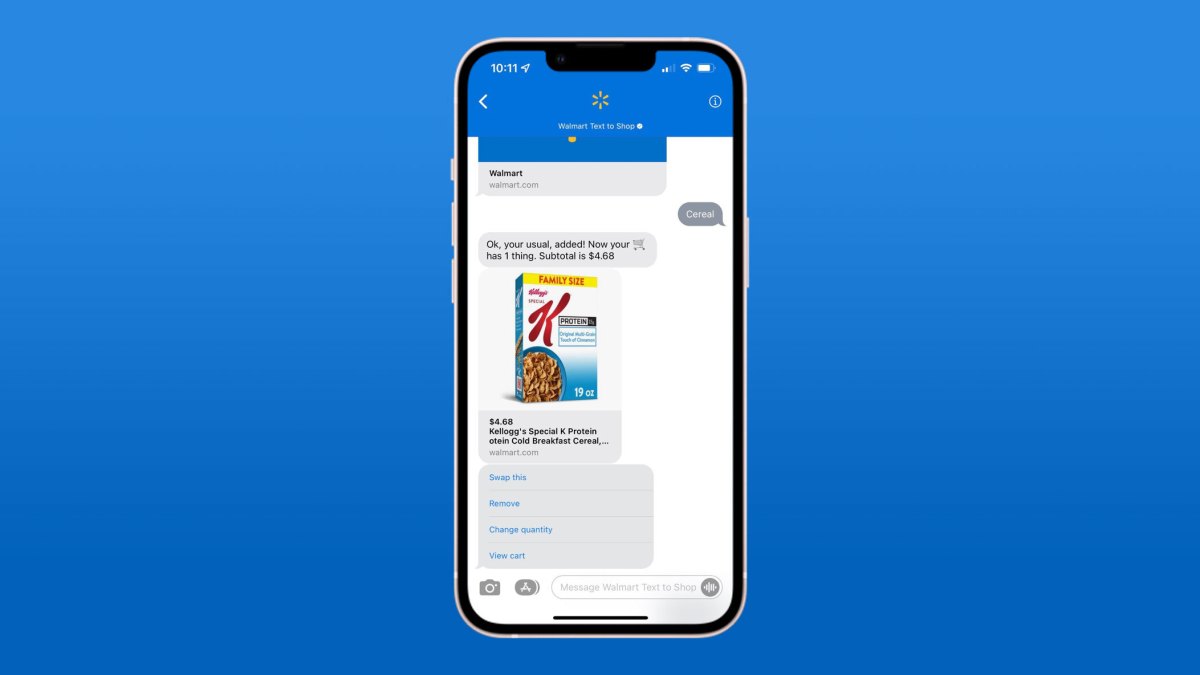
Novo Nordisk’s campaign “It’s Bigger Than Me,” with actor Queen Latifah as its face, has drawn particular criticism. Through it, the company is trying to align itself with the talking points of fat acceptance—eliminating weight stigma and bias and shattering the misconception that obesity is simply a lack of willful control—while at the same time selling a drug that has the goal of making fat people smaller. “By saying that if you take away the fatness, you’re giving them the chance to thrive, you’re not—you’re just making the person smaller, and you’re selling them smallness as a gateway out of oppression,” says Marquisele Mercedes, a doctoral student in public health at Brown University.
Yet these concerns are opposed by an obvious truth: Anti-obesity drugs are effective at tackling what is a complicated condition. While the underpinnings of obesity remain elusive, a colliding consensus among researchers has landed on one irrefutable fact: Obesity is not a physical manifestation of an absence of willpower. Research has proven, repeatedly, that dieting doesn’t work to reduce weight and keep it off. Obesity is a complex, entangled mishmash of biological and environmental factors that scientists have yet to fully solve and which can’t be boiled down to the simple matter of calories in, calories out. “That concept is wrong,” says Francesco Rubino, a professor of metabolic surgery at King’s College London. “It’s not true that obesity is the consequence of too much energy.”
Having working drugs that can step in where other interventions have failed will offer important health benefits for some. Obesity raises the risk of a number of debilitating and deadly conditions, including heart disease, diabetes, high blood pressure, stroke, and certain forms of cancer. These drugs could even help solve the mystery of the root causes of weight gain, Rubino says. On top of a reduced urge to eat, people who take semaglutide appear to have a lowered impulse to partake in dopamine-fueled behaviors, like drinking booze or shopping, according to David Macklin, a doctor who has treated many patients with the drug.
But these treatments aren’t intended for the masses. They are indicated for a specific group of patients: people with a body mass index of 30 kg/m², the clinical definition of obesity, or for people who have a BMI of 27 kg/m² or higher (and so are classified as overweight) if they have another weight-related condition that threatens their health, such as high blood pressure. (It’s worth mentioning that BMI, the diagnostic tool most commonly used globally to determine obesity, has been shown to be a flawed and discriminatory health metric.)