Summary: A large-scale study by the SSPsyGene consortium aims to unravel the genetic roots of neurodevelopmental and psychiatric disorders by systematically mutating 250 high-risk genes in human stem cells.
Estimated reading time: 5 minutes
A groundbreaking research initiative is shedding new light on the genetic underpinnings of mental illness. The SSPsyGene consortium, launched by the National Institute of Mental Health (NIMH) in 2023, brings together top researchers from across the United States to investigate the role of high-risk genes in neurodevelopmental and psychiatric disorders (NPDs).
NPDs, including schizophrenia, bipolar disorder, autism, and depression, affect millions worldwide and often lack effective treatments. While hundreds of “risk genes” have been identified, their specific contributions to these disorders remain largely unknown. The SSPsyGene project aims to change that by systematically studying 250 selected high-risk genes.
Why it matters: This research could lead to a deeper understanding of how genetic variations contribute to mental illness, potentially paving the way for more targeted and effective treatments. By creating a comprehensive resource of mutated stem cell lines, the project opens up new avenues for studying these disorders in human brain cells, rather than relying on less relevant cancer cell lines or animal models.
Unraveling the Genetic Puzzle of Mental Illness
David Panchision, Chief of the Developmental and Genomic Neuroscience Research Branch at NIMH and spearhead of the SSPsyGene program, explains the current challenge: “Very little is known about the basic function of most of these genes, and what we do know often comes from work in cancer cell lines rather than brain cell types. As such, we still don’t have a clear understanding of how alterations in these genes may work individually or in combination to contribute to neurodevelopmental and psychiatric disorders.”
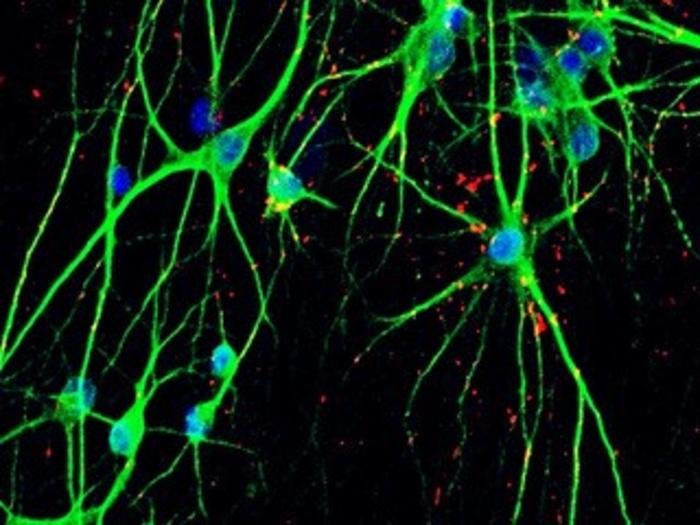
To address this knowledge gap, researchers have developed an innovative method for mutating NPD risk genes in human stem cells on a large scale. This technique allows them to create modified cells where a selected risk gene no longer produces a functional protein. These modified stem cells can then be transformed into neurons and other brain cells, providing a simplified, lab-based model of how genetic mutations might affect the human brain.
A Collaborative Effort to Decode Mental Illness
The SSPsyGene consortium brings together experts from various fields, including geneticists, neuroscientists, and stem cell biologists. Key contributors to the project include Jubao Duan from Endeavor Health (formerly NorthShore University Health System) and the University of Chicago, and Zhiping Pang from Rutgers University.
In the initial phase of the project, the team successfully tested their method on 23 NPD risk genes. The results of this work, published in the journal Stem Cell Reports, demonstrate the feasibility of their approach and lay the groundwork for studying a much larger number of genes.
From Lab to Clinic: Potential Impact on Mental Health Treatment
The ultimate goal of the SSPsyGene project is to generate a comprehensive set of mutated stem cell lines covering 250 high-risk genes associated with NPDs. These cell lines will be made available to researchers worldwide, creating a valuable resource for the scientific community.
By studying these modified cells, researchers hope to gain insights into how specific genetic mutations contribute to the development of mental illnesses. This knowledge could lead to:
- Better diagnostic tools for identifying individuals at high risk for NPDs
- New targets for drug development
- More personalized treatment approaches based on an individual’s genetic profile
Panchision expresses optimism about the project’s potential impact: “The hope is that this collaborative work will generate a highly impactful resource for the neuroscience and psychiatric research community.”
Challenges and Future Directions
While the SSPsyGene project represents a significant step forward in mental health research, several challenges remain:
- Complexity of gene interactions: Mental illnesses often result from complex interactions between multiple genes and environmental factors. Studying individual genes in isolation may not capture the full picture.
- Translating findings to clinical applications: Moving from lab-based discoveries to real-world treatments is a long and complex process.
- Ethical considerations: As our understanding of the genetic basis of mental illness grows, it raises important ethical questions about genetic testing and potential stigmatization.
Despite these challenges, the SSPsyGene consortium’s work offers hope for millions affected by NPDs. By systematically investigating the role of high-risk genes, researchers are laying the foundation for a new era of mental health research and treatment.
Quiz:
- What is the main goal of the SSPsyGene consortium?
- How many high-risk genes does the project aim to study in total?
- What type of cells are researchers using to model the effects of genetic mutations?
Answer Key:
- To characterize the genetic origins of neurodevelopmental and psychiatric disorders (NPDs) by studying high-risk genes.
- 250 selected high-risk genes.
- Human induced pluripotent stem cells (hiPSCs) that can be turned into neurons and other brain cells.














































![‘First Wives Club’ Season 3 Gets Release Date on BET+, Trailer [VIDEO] ‘First Wives Club’ Season 3 Gets Release Date on BET+, Trailer [VIDEO]](https://tvline.com/wp-content/uploads/2022/10/First-Wives-Club-Jill-Scott-BET-Plus.jpg?w=620)






