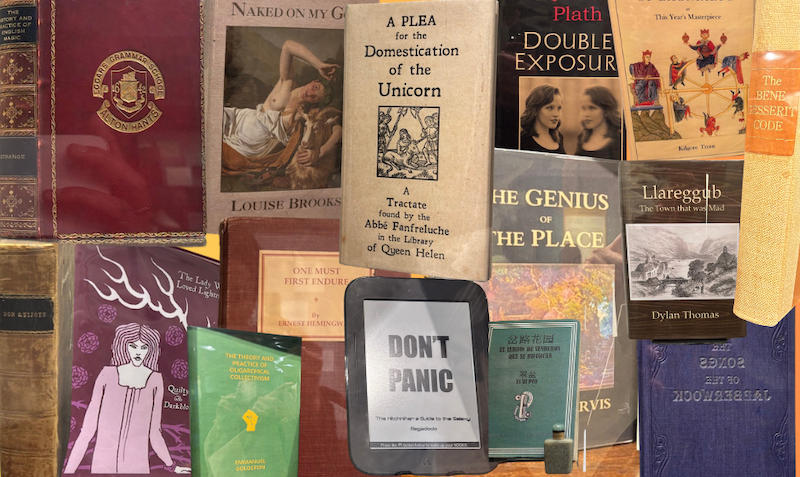
Aggregated clumps of the protein alpha-synuclein (brown) and antibodies (green)
BIOLUTION GMBH/SCIENCE PHOTO LIBRARY
A drug that targets a build-up of proteins linked to Parkinson’s disease could slow the progression of motor symptoms in people with advanced forms of the condition. Although this shows promise to be a disease-modifying treatment for Parkinson’s, it is unclear whether the drug actually clears the proteins from the brain.
The accumulation of a misfolded protein called alpha-synuclein in the brain has long been considered the underlying cause of Parkinson’s. This leads to the loss of neurons that produce the neurotransmitter dopamine, which is involved in motor control.
While some existing treatments aim to ease these symptoms by improving dopamine levels in the brain, their long-term effects are limited. So far, there are no approved disease-modifying therapies that halt or slow the progression of Parkinson’s.
In an effort to combat this, Gennaro Pagano at Swiss pharmaceutical company Roche and his colleagues recruited 316 people who were thought to have early-stage Parkinson’s disease. Of these individuals, 105 received intravenous infusions of a placebo, while 211 had infusions of the Roche drug prasinezumab at either a low or high dose, administered every four weeks over one year.
Prasinezumab is an antibody that is designed to bind to aggregated clumps of misfolded alpha-synuclein in dopamine-producing neurons. “It is hypothesised that prasinezumab may reduce neuronal toxicity, prevent cell-to-cell transfer of pathological alpha-synuclein aggregates and slow disease progression,” says Pagano.
While the results of the trial initially suggested that the antibody had no meaningful impact, the team then realised it may be effective among the trial participants with more severe Parkinson’s.
These individuals had rapid eye movement sleep behaviour disorder, where people act out intense and often violent dreams, which is common in Parkinson’s; were taking drugs called MAO-B inhibitors to manage their symptoms; or had been rated by their specialist as being at stage two out of five on a symptom scale, with a higher number indicating greater severity.
An additional analysis showed that both low and high doses of the drug had a greater effect among the severe participants specifically than seen in the initial work. Compared with taking a placebo, it significantly reduced the rate at which participants’ motor symptoms worsened over the year-long period.
For example, based on a Parkinson’s disease rating scale for motor symptoms, those on MAO-B inhibitors who then received placebo infusions scored 6.82 at the end of the year, while those taking both the inhibitors and prasinezumab scored 4.15.
“The results imply that in a faster-progressing population, where the degree of worsening over time is greater, there is an increased likelihood of a potential treatment effect,” says Pagano. This could be because people with more rapidly progressing Parkinson’s have higher amounts of misfolded alpha-synuclein in their brains, so would probably benefit more from a drug that potentially clears the protein.
However, Pagano says it wasn’t possible to assess exactly what was happening in any of the participants’ brains because the researchers lacked a biomarker that would have enabled them to monitor how their levels of misfolded alpha-synuclein may be changing.
Vinata Vedam-Mai at the University of Florida Health says a limitation of the study is that it didn’t assess whether alpha-synuclein was being cleared from the brain. Without this, the results can’t conclusively show prasinezumab is disease-modifying, she says. Vedam-Mai says she would also like to see longer-term data to better gauge the drug’s safety and efficacy. No serious adverse events took place in the latest trial.
Researchers could also investigate whether prasinezumab is effective in people with milder Parkinson’s disease when taken over a longer period, says Pagano.
Topics: