The people who seek out endocrinologist Domenica Rubino have tried again and again to lose weight. Diets of all kinds. Exercise regimens. Health-tracking apps. Some have turned to gastric bypass surgery, lost scores of pounds but then regained them. Many patients have medical problems related to severe obesity, including diabetes, fatty liver disease, hypertension, polycystic ovary syndrome, sleep apnea and painful arthritic joints. Rubino, director of the Washington Center for Weight Management and Research in Arlington, Va., says that for years she had relatively few tools to help them. That changed with the recent advent of medications directly targeting the brain-gut axis that regulates appetite. “We are finally able to help people lose weight in the ranges that help the complications of obesity,” Rubino says.
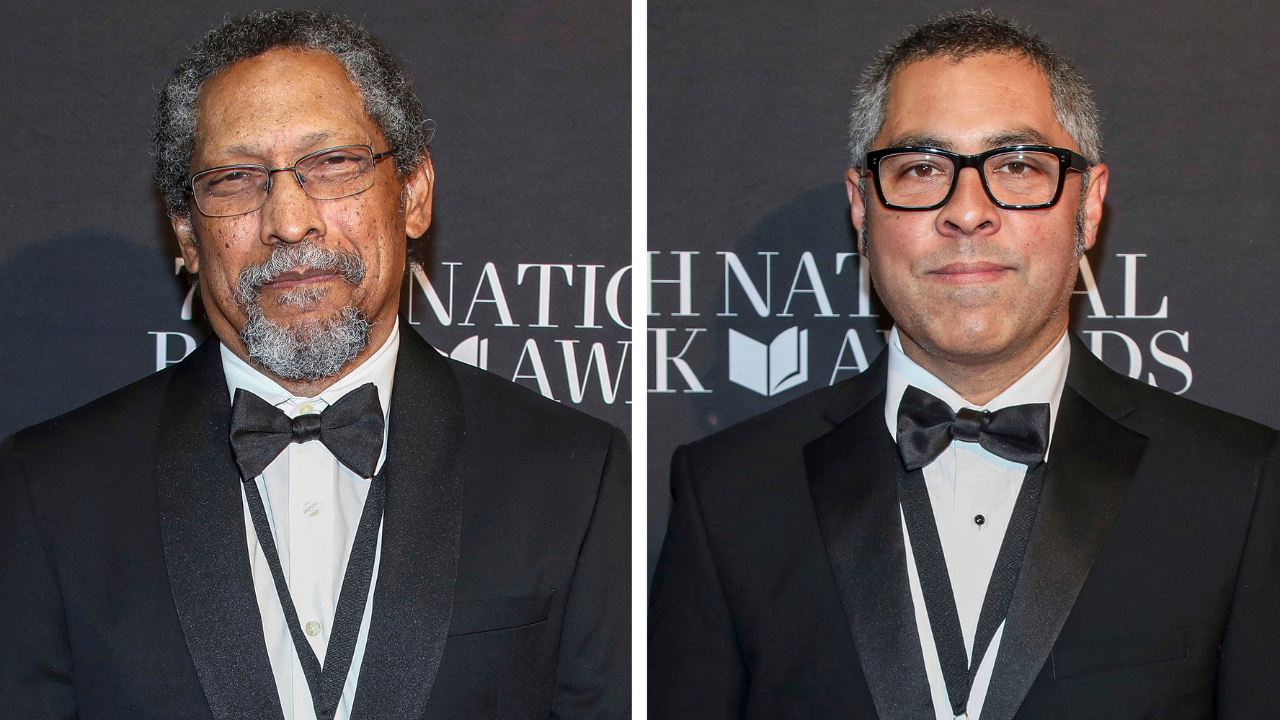
The medication generating the most excitement is a weekly injectable drug called semaglutide (brand name: Wegovy). It was approved in June 2021 for treating people with a body mass index in the obese range or just under that range but with weight-related health issues. A study involving 1,961 such individuals published last year in the New England Journal of Medicine found that, on average, people taking semaglutide lost 14.9 percent of their initial body weight over 68 weeks compared with just 2.4 percent for a group receiving placebo injections. Such results are about double what older weight-loss drugs achieve, says Robert Kushner of Northwestern University, one of the study’s principal investigators. Evidence from the trial suggests that along with weight loss come reductions in blood pressure, blood glucose and unhealthy lipids, as well as C-reactive protein (a measure of inflammation).
Kushner emphasizes the drug is not just for weight loss but to reduce the associated risk of chronic illnesses. “We want to be sure our patients are getting healthier, not just thinner,” he says.
Semaglutide is widely seen as a breakthrough—“a new paradigm for the hormonal treatment of obesity,” as Kushner puts it. The medicine mimics a gut hormone called glucagon-like peptide-1 (GLP-1) that acts on the pancreas to increase insulin production, on the stomach to slow emptying, and on the brain to turn down appetite and signal satiety. Patients can eat less and not be bothered by hunger and cravings. Other medications are in development that combine two or three hormones involved in appetite.
The hitch is that these drugs must be used throughout life, much like diabetes medications, or else the benefits are lost. In fact, a 2021 study led by Rubino found that people on semaglutide regain weight when the drug is stopped. The premise of such treatments is that serious obesity is not a transitory condition related mainly to behavior and environmental factors, as many people see it. Rather, in the view of the National Institutes of Health and the American Medical Association, it is a chronic, relapsing disease—one that disrupts multiple physiological systems.
Still, the prospect of a lifetime of weekly injections to maintain weight loss raises a number of questions, beginning with safety. Anything that alters functions as fundamental as metabolism and energy balance can have significant side effects. The diet pill Fen-Phen, now banned, caused heart valve damage, for instance. Most people on semaglutide experience nausea and diarrhea, but these are usually mitigated by starting them on a low dose. In the New England Journal of Medicine study, only 4.5 percent of semaglutide recipients dropped out because of gastrointestinal symptoms. Kushner also points out that a lower-dose version of semaglutide, marketed as Ozempic, has been used for type 2 diabetes for more than four years, “and the safety profile is good.” But a higher dose taken over many decades could be another matter.
Cost is also an issue for the weight-loss drug and will likely be a problem for similar medications. The price is $1,349 a month. Insurance coverage is spotty, and Medicare does not pay for it. Yet demand is so strong the drugmaker, Novo Nordisk, can’t keep up. “We’ve been asked to hold off starting new patients,” Kushner says.
The rush to embrace a lifelong injectable drug makes some obesity researchers nervous. “As someone who studies lifestyle interventions, I feel that our health-care system is just focused on treatment and not prevention,” says Krista Varady, a professor of nutrition at the University of Illinois, Chicago. “We just wait for people to get sick so we can sell them things like drugs.”
Prevention would undoubtedly be better, Rubino agrees, but many of her patients are already ill. Her team always promotes a healthier diet and more exercise, she says, and “the medicines provide physiological support for those changes.”