A Scottish woman named Joy Milne made headlines in 2015 for an unusual talent: her ability to sniff out people afflicted with Parkinson’s disease, a progressive neurodegenerative illness that is estimated to affect nearly a million people in the U.S. alone. Since then a group of scientists in the U.K. has been working with Milne to pinpoint the molecules that give Parkinson’s its distinct olfactory signature. The team has now zeroed in on a set of molecules specific to the disease—and has created a simple skin-swab-based test to detect them.
Milne, a 72-year-old retired nurse from Perth, Scotland, has hereditary hyperosmia, a condition that endows people with a hypersensitivity to smell. She discovered that she could sense Parkinson’s with her nose after noticing her late husband, Les, was emitting a musky odor that she had not detected before. Eventually, she linked this change in scent to Parkinson’s when he was diagnosed with the disease many years later. Les passed away in 2015.
In 2012 Milne met Tilo Kunath, a neuroscientist at the University of Edinburgh in Scotland, at an event organized by the research and support charity Parkinson’s UK. Although skeptical at first, Kunath and his colleagues decided to put Milne’s claims to the test. They gave her 12 T-shirts, six from people with Parkinson’s and six from healthy individuals. She correctly identified the disease in all six cases—and the one T-shirt from a healthy person she categorized as having Parkinson’s belonged to someone who went on to be diagnosed with the disease less than a year later.
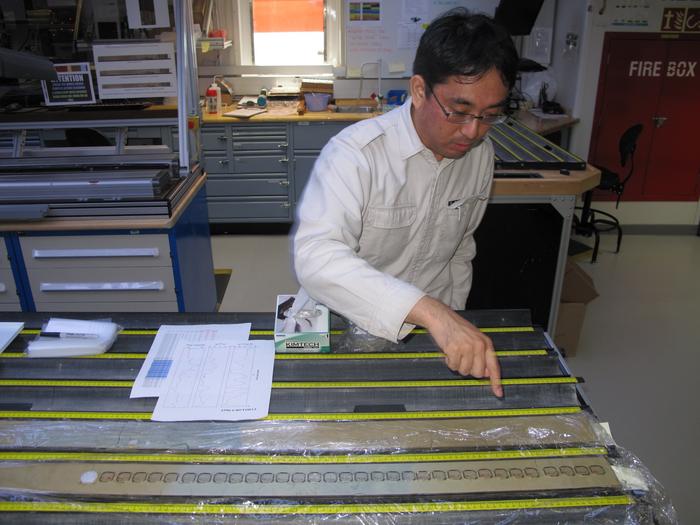
Subsequently, Kunath, along with chemist Perdita Barran of the University of Manchester in England and her colleagues, has been searching for the molecules responsible for the change in smell that Milne can detect. The researchers used mass spectrometry to identify types and quantities of molecules in a sample of sebum, an oily substance found on the skin’s surface. They discovered changes to fatty molecules known as lipids in people with Parkinson’s.
In their latest study, published on September 7 in the American Chemical Society journal JACS Au, the researchers revealed the results of using a simple skin-swab-based test to detect the lipid signature that is indicative of Parkinson’s. By comparing sebum samples from 79 people with Parkinson’s and 71 people without the illness, the team zeroed in on a set of large lipids that could be detected in a matter of minutes using a special type of mass spectrometry in which substances are rapidly transferred from a swab to an analyzer using just a piece of paper.
“I think it’s a very promising set of biomarkers,” says Blaine Roberts, a biochemist at Emory University, who wasn’t involved in the work. He adds that one of the big open questions that remains is how exacting this test can be. While the authors of the September 7 study reported the detailed chemical profile of the unique Parkinson’s signature, they did not include an assessment of its accuracy. According to Barran, based on not-yet-published data, their test appears to be able to determine whether an individual has Parkinson’s with more than 90 percent accuracy.
Tiago Outeiro, a neuroscientist at the University of Göttingen in Germany, who was not involved with the research, says the sebum-based swab test is novel and has clear advantages, such as the ease of sample collection. Outeiro wonders whether people with diseases that share symptoms and pathologies with Parkinson’s disease, such as multiple system atrophy, also have similar chemical markers.
The team is now working with local hospitals to determine whether this sebum-based test can also be conducted in clinical labs—a key step toward determining whether it can be used as a diagnostic tool. Ultimately, Barran says, the hope is to use the test to help identify individuals who have been referred to their neurologists by their general practitioner for suspected Parkinson’s so they can receive a faster diagnosis. Currently, there are thousands of people waiting to see a neurologist in the U.K.’s National Health Service, and it will take an estimated two years to clear that list, Barran says. A skin-swab test could enable those patients to mail in skin swabs to be analyzed in the hospital laboratory and pinpoint those who need help most urgently. Barran’s research team is approaching people on the waiting list to see if they are willing to take part in a trial to see whether such skin-swab tests could prove effective in helping to speed up the triage process.
Barran and her colleagues are also collaborating with a group at Harvard University to determine whether sebum-based biomarkers are detectable in people who have constipation, a reduced sense of smell or other early signs of Parkinson’s but have not yet received a diagnosis.
Milne has inspired groups elsewhere to search for biomarkers based on the disease’s olfactory signature. This year researchers in China published a paper describing an electronic nose—an artificial-intelligence-based sensor modeled after the olfactory system—that sniffs out molecules present in the sebum of patients with Parkinson’s disease. Other groups in China, the U.K. and elsewhere have also been training dogs to sniff out the disease.
Parkinson’s may not be the only disease Milne has a nose for. She’s also reported noticing a unique smell in people with Alzheimer’s, cancer, and tuberculosis and is working with scientists to see whether a specific olfactory signature of those diseases can be deduced.
For Milne, the hope is that this work will ultimately benefit patients with these conditions. “My husband suffered from [Parkinson’s] for 21 years after his diagnosis, but he had it many years before that,” Milne told Scientific American in 2015. “I would like to see that people don’t suffer the way he suffered.”