“You’ve been here before, two years ago.” The receptionist’s voice was bright and cheerful.
“Right, for my hip.”
I heard the smile in her voice. “We received your doctor’s referral for your shoulder. But it’s office policy that you stick with the same physician you’ve seen in the past.”
My primary care doctor had wanted me to see Dr. M—a shoulder specialist. She was concerned I had torn my rotator cuff.
It was easier for her to remain demure, polite, and well-behaved throughout the process.
The receptionist’s sweet tone prompted a similarly polite response from me. “Okay.”
“Now, Dr. B is getting ready to head out on vacation. So the earliest I can get you in is September 20th. Will that work for you?”
I stared at my calendar.The pain of the past two months compelled me to protest an appointment that loomed a month out. I wanted to request we stick with the referral of Dr. M that had been sent over. Common sense dictated that the odds of both physicians being out of the office simultaneously was slim. I stood a good chance of being seen sooner, and Dr. M was a shoulder specialist; Dr. B had addressed a hip issue for me. But I kept hearing the words “office policy” over and over in my head. And I didn’t want to be seen as a difficult patient.
“That’s fine. Thank you.”
I couldn’t speak up. Like so many women, I’d learned accommodating behavior throughout my childhood. Mixed with my parents’ lessons to stand up for myself were conflicting messages to respect authority figures—regardless of what they said—and always keep my voice moderated and calm. I’d soaked up the warning that vocally resisting the status quo was unacceptable.
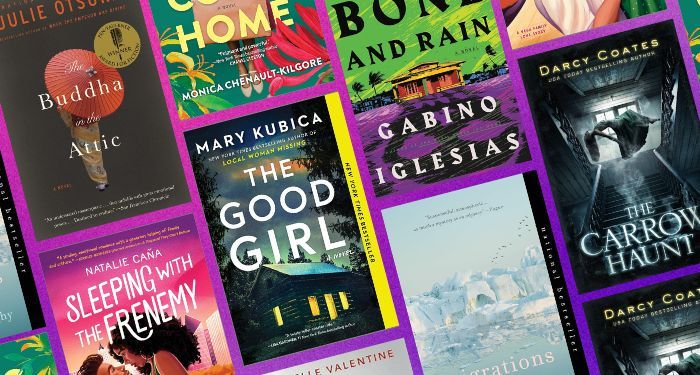
In her tragicomic memoir, Hysterical, Elissa Bassist brings this female programming into the light. She demonstrates how everything around women, from the television they watch to their political stance to the way they’re educated, influences their behavior and how they become quieter as they age—regardless of how outspoken they may appear. The pressure becomes overwhelming, creating an enforced silence that turns women into automatons, fearful of saying anything lest an accusation of stepping out of line or becoming a “problem” emerges. As she writes, “Don’t talk back. Don’t tell. Don’t say this (or that). Don’t draw attention. Don’t be difficult. Be pleasant. Be who everyone needs you to be.”
Bassist’s realization of her own silence arose when she started experiencing dreaded non-specific medical symptoms. Chasing the source of various pains throughout her head and abdomen sent her from one specialist to another, leading to a potentially fatal condition of hyponatremia, or low blood sodium, as each prescribed and adjusted medication. The entire time, she was struggling with undiagnosed OCD and mismanaged depression stemming from an incident of sexual abuse. But it was easier for her to remain demure, polite, and well-behaved throughout the process, wanting to avoid the impression of being a “stressed-out hypochondriac,” the expectation of which was drilled into her from her cultural and educational experiences.
And I was no different.
“I spoke in ‘the good female patient voice’: the pleasant and accepting and grateful voice, the voice that wasn’t too assertive or too blunt or too cold, the voice that didn’t ask too many questions or follow up too frequently, and especially the apologetic voice,” Bassist writes in a description of her doctor visits that mimicked mine to a T.
A stereotype has arisen that dramatic women exaggerate their pain to get attention.
I didn’t walk in and complain that I wanted to scream whenever I washed my hair. That I was contemplating shaving my head to prevent the electric shocks that ran down my shoulder when I attempted more than running a comb through my hair. I didn’t mention the embarrassment of needing my husband’s help putting my bra on because my arm refused to bend behind my back, leaving me wailing helplessly in the middle of the bedroom.
Instead, I quietly explained to my primary care doctor that I was having trouble sleeping at night. I bit my tongue so I wouldn’t curse aloud as she manipulated the joint to ascertain how far I could move. I agreed with her treatment plan and waited six days to call the office and report that the steroids weren’t working. I felt an inexplicable need to stay as calm as possible and not speak of my pain too much. I was afraid that if I told her how much agony I was actually in—that it felt like a blade wedged between the bones—she’d stop taking me seriously. And that pressure kept me quiet.
And I loved my PCP. She listened to me and took my concerns seriously. It had taken me two decades to find her while I suffered with doctors who dismissed every word that came out of my mouth. But I couldn’t get past the signs on the door warning patients of the new pain management policies: referral to a pain specialist, the dangers of narcotic prescriptions, and a refusal to prescribe narcotics without a “significant reason.” The threatening language made me swallow any words related to pain.
I, and other women like me, have learned to stay silent about our medical problems. Even when it means we receive poor care as a result. As Alyson J. McGregor wrote in Sex Matters: How Male-Centric Medicine Endangers Women’s Health and What We Can Do About It, “The more vocal women become about their pain, the more likely their providers are to ‘tune them out’ and prescribe either inadequate or inappropriate pain relief.” A stereotype has arisen that dramatic women exaggerate their pain to get attention. And that’s led to longer wait times at the ER (up to 33% longer) than men who present with similar symptoms. A problem that only reinforces the need to stay quiet and endure in silence.
Women, through both an evolutionary nature and our nurturing process by parental figures, are accommodating. (At least the majority of us; a lucky few manage to escape the programming) As Bassist puts it, “The disease to please is our birth defect, and then we’re brought up to be obliging, reassuring, and non combative. To refuse is ‘demanding,’ ‘hostile,’ and ‘hideous,’ and we should not hurt someone else’s feelings by expressing our own.” I was caught in the quandary of not wanting to make too much of my pain and wanting to acquiesce to the orthopedic office’s policy. My only real option was to agree. And the price was my voice.
Like Bassist, I was determined to “suffer less—invisibly or with a smile—to not provoke or inconvenience or frustrate anyone, ever.”
Until the orthopedic office called again.
“Ms. Kennedy, we need to push your appointment back. Dr. B won’t be available on September 20th. Could you come in October instead?” The receptionist was as polite as always. And I could hear the expectation of my usual accommodation in her tone.
But my common sense wasn’t ready to offer quiet acquiescence. I’d accepted the September appointment while the doctor went on vacation. Now I needed a further delay? Had he decided to extend his trip? Contracted COVID wherever he’d gone? Was he aware of my referral and that I’d been dealing with intense shoulder pain for over two months?
The pause on the other side of the line felt like an indictment of my tone.
When a doctor fails to explore the full battery of testing or refuses to sit down and listen to a patient, the patient has the right to speak up for themselves. No one knows their body better, and that’s especially true for women. Yet females, in particular, are often reluctant to say anything. The engrained lessons that authority figures, such as doctors, know far better than we do make it challenging to ask questions. And that fuels the 20% of women who report that they feel a doctor ignores or dismisses their symptoms, compared to only 14% of men. It was why I hadn’t insisted on an appointment with Dr. M in the first place, leaving me in this situation.
I felt like Bassist was sitting beside me, her hand in mine. I took a deep breath to quell my shaking. “It’s been over two months since I started having problems. What’s the soonest he can see me?”
The pause on the other side of the line felt like an indictment of my tone, and I wanted to crawl under the desk. But my shoulder was already aching, and I pressed my lips together to hold in the need to apologize. The receptionist’s voice was a little quieter but still cheerful. “Would October 6th work?”
“Yes.” I hesitated. “Could you put me on a waitlist in case there’s an earlier cancellation?”
“Of course.”
When I hung up the phone, I felt like I’d run a marathon. I could barely catch my breath. On the one hand, an oppressive weight urged me to call back and apologize for my “behavior.” But on the other hand, I felt a sudden freedom. I’d spoken up—however small the words had been. It was the most rebellious act I’d ever attempted with a medical professional. And I was caught between feeling gloriously defiant and horrified that I dared to ask for “special consideration.”
“Women who feel and express feeling are associated with madness and sickness until ‘vocal’ is a symptom,” Bassist writes. Part of me was convinced the receptionist was, at that moment, making a note in my chart that I was a “difficult patient.” I had visions of my appointment devolving into a catastrophic nightmare of tears and yelling. But I wondered how much of that was due to the ingrained thoughts and impressions of forty-plus years of social and cultural teaching. As Bassist demonstrates in Hysterical, we’re so conditioned to accept the image of an outspoken and confident woman as “hysterical” that it makes it almost impossible for any woman to break free of the mold, regardless of what she attempts to say—whether it’s to declare herself a victim of sexual assault or demand proper medical care.
“It wasn’t my voice that would obliterate me. It was my silence.” Bassist’s words wouldn’t leave me as I walked into the orthopedist’s office. I could repeat my performance with my primary doctor and downplay the agony impacting my life. (In short, I could behave the way society expected). Or I could speak up and tell Dr. B exactly how badly the pain was making me feel. Even if it risked making me sound like a vocal, hysterical woman.
“It’s nice to see you again, Ms. Kennedy,” Dr. B said, walking into the room with a wide smile.
I felt the moment stretching, his expression expecting the usual polite response to his greeting. During my previous visits, I always responded with an immediate smile and automatic cheerful remark. It was what the medical team had come to expect from me.
But my arm felt like it had been torn out of the socket, courtesy of the preceding x-rays. And I’d waited over a month to see him. I took a deep breath, folded my hands in my lap to disguise their shaking, and looked him in the eye. “Not really. I’ve been in pain since mid-July, and it keeps getting worse. And I had to wait an extra two weeks to see you.”
I let my silent winces speak for me, not wanting to be “difficult” or “dramatic.”
The smile vanished from his face. I watched him exchange a look with the transcriptionist. “Well, let’s take a look at that shoulder then.”
Before, I allowed doctors to bend and twist my arm as far as they wanted, regardless of how much pain it caused. I let my silent winces speak for me, not wanting to be “difficult” or “dramatic.” But as he manipulated my shoulder, attempting to bend it into the positions that sparked the sharpest pains, I said, “No” in a firm voice. He stopped immediately, and I exhaled in relief.
“I don’t think you’ve torn your rotator cuff, but I do think you have adhesive capsulitis—frozen shoulder. I’d like to start you with physical therapy for four weeks. If there’s no improvement in the pain in that time, I’ll order an MRI. And we’ll proceed from there.” He paused, lifting an eyebrow. “Does that sound okay to you?”
I couldn’t remember the last time a doctor had checked with me about a treatment plan. Usually, they rattled it off and left the room—whether I agreed or not. I asked a few more questions about the condition, and he stayed to answer them. He didn’t show any inclination to hurry to his next appointment. My body relaxed, and I found myself smiling for the first time. “Let’s go ahead with the physical therapy.”
“If you have any other questions before your recheck, just give me a call.” He reached out and shook my hand.
While it felt like a battle to get past the pressure of sitting in silence, I had managed to speak up.
I walked from the office feeling confident. I’d been an active participant in my care for the first time. And while it felt like a battle to get past the pressure of sitting in silence, I had managed to speak up. The accomplishment eased the tension in my shoulders, taking away some of the pain.
“In a perfect world–not a man’s world or a woman’s world–I’d speak again easily and often, without overthinking or having to hype myself up in the mirror beforehand,” says Bassist. Reading Hysterical shifted the way I approached my typical silences. Instead of hesitating over how my words would be perceived, I started to think of how the fallout of not speaking felt. Did I want to live in a world where I was unheard and unseen? Or did I want to take the chance that saying something might cause a frown but might ultimately lead to a better experience?
The conditioning women experience throughout their lives is intense. And so is the fight to break free. It’s why Bassist has made her call to arms so powerful: “Risk demanding care. Risk a voice that doesn’t demure, a voice that is difficult, unaesthetic, charged, forthright, sappy. Risk it, or risk living a half-a-life person.”