COVID has been haunting humans for four and a half years, and experts agree there are no signs that it will disappear. So even though we would all like to forget about it, we should remain vigilant to protect our health. Here’s a quick guide to the latest information about COVID rates, treatments and upcoming vaccines.
COVID Rates Are Very High
Exact case counts are no longer being tracked, but current indicators show that COVID infections in the U.S. are widespread. In the week ending on August 10, nearly one in five COVID tests reported to health departments was positive, and one in 40 people who visited an emergency department was diagnosed with COVID, according to data from the Centers for Disease Control and Prevention. Nearly 2 percent of all deaths reported during that week were caused by the disease.
On supporting science journalism
If you’re enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
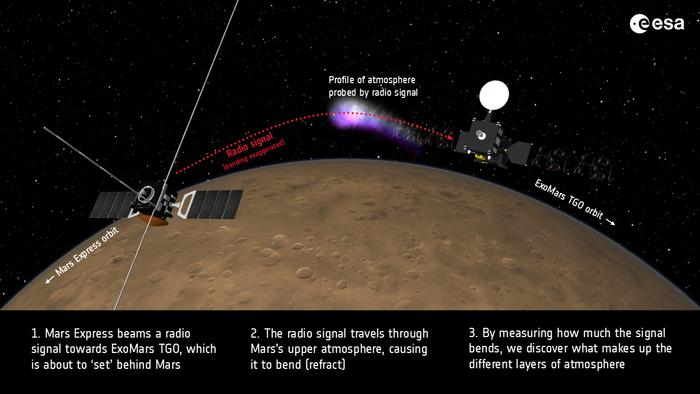
Wastewater analysis is one of our best tools for understanding what’s happening with COVID right now. These surveys measure viral RNA shed into community sewer systems—a reporting metric that isn’t skewed by changes in testing practices.
And the latest data show concentrations of the COVID-causing virus SARS-CoV-2 in those samples are “quite high—they’re actually, at this point, the highest that we have seen for a summer surge in the past several years,” says Marlene Wolfe, an environmental microbiologist at Emory University. That said, current rates remain lower than the concentrations seen during previous winter peaks.
Viral concentrations show some variability among communities, but levels are currently high across the nation, says Wolfe, who is also a program director at WastewaterSCAN, a nonprofit organization that analyzes wastewater samples from about 150 sites nationwide for a range of infectious diseases to understand their prevalence. (The CDC also runs a wastewater monitoring network, which is likewise detecting very high levels of COVID nationwide.)
The past three weeks of data, however, show relatively stable concentrations after steady rises throughout the summer, leading Wolfe to hope that rates might begin to fall soon—although that doesn’t mean we’re in the clear. “Even if we do start to see that downturn, these concentrations are still very high, and that represents a lot of people who are infected and sick right now,” Wolfe says.
COVID Is Less Deadly; Long COVID Is Taking a Toll
New long-term studies are also helping us better understand the pandemic’s full ramifications over time.
Recently released provisional CDC data show that deaths from COVID fell dramatically from 2022 to 2023: the disease dropped to the 10th leading cause of death in latter year, whereas it had previously been the fourth.
Despite this improvement, a new analysis published this month shows the heavy toll of long COVID worldwide. The report estimated that some 400 million people were diagnosed with the condition between 2020 and 2023 and that it has conservatively cost around $1 trillion each year. “Those numbers are huge,” says Ziyad al-Aly, a clinical epidemiologist at Washington University in St. Louis and chief of research at the Veterans Affairs St. Louis Health Care System, who co-authored the new paper. “It’s a gloomy picture.”
Some people who contract long COVID do fully recover, but they are far from the majority. Many continue to struggle a year after infection, al-Aly notes. And while research on the condition has progressed in the past couple of years, including through the National Institutes of Health’s Researching COVID to Enhance Recovery (RECOVER) Initiative, it’s still lagging, he says.
Masks and Vaccination Can Help
The same prevention tactics remain available and effective: Vaccines can reduce your odds of serious infection. And wearing a mask can help you to avoid catching the virus—or giving it to those around you, should you be infectious.
Infectious disease experts say waning immunity from previous vaccination or infection can make people susceptible to catching COVID. But fortunately updated vaccines are coming soon that will provide protection against the latest variants of SARS-CoV-2. The companies Pfizer and Moderna will be releasing new mRNA vaccines tailored to the currently circulating variant KP.2. Meanwhile Novavax is producing a traditional protein-based vaccine tailored to another variant called JN.1. Both of these variants are offshoots of the Omicron variant. As of August 20, KP.2 and another variant called KP.3 are currently the most dominant forms in the U.S. These variants are all very closely related, and the vaccines are expected to provide equally strong immunity to them.
The CDC recommends the updated COVID vaccines for everyone older than the age of six months. The Food and Drug Administration signed off on the Pfizer and Moderna vaccines on August 22 and is expected to do the same for the Novavax vaccine soon. Pfizer and Moderna representatives have said their vaccines should be available within days. As preventive care, the new vaccines should be fully covered by insurance, says Archana Chatterjee, a pediatric infectious disease expert at Rosalind Franklin University. People who do not have insurance face additional hurdles because the federal government ended a program that was meant to support access to COVID vaccines through the end of this year. Chatterjee suggests that such individuals should research manufacturers’ access programs to receive a shot at no or reduced cost. Children can also access vaccines free of cost through the federal government’s Vaccines for Children Program.
As with previous iterations, the new COVID vaccines are meant to lower the likelihood of serious disease—the type of infection that can hospitalize or even kill people. Although it’s too early to know how the three brands of vaccines will perform against one another, Chatterjee says, she doesn’t want people to get hung up on the different options and just get a vaccine. She also encourages people to get vaccinated early rather than waiting until closer to an expected winter surge. While a vaccine’s immune boost is strongest in the two to three months following injection, it persists long after.
“My advice to people is: get the updated vaccine as soon as it’s available,” Chatterjee says. Most of all, she hopes more people get the new vaccine than did so last year. Only one in 10 people who were hospitalized with COVID in the past year had received the newest shot, and as of May, just one in five U.S. adults had received a 2023–2024 vaccine—a number Chatterjee calls “deplorable.” “This is not going to control this disease,” she says, adding that this year we need to do better.
People who are at particularly high risk of serious COVID infections will have the opportunity to get an additional shot a few months after their first dose of the new vaccine to provide a further boost to their immune system. And people with compromised immunity will also have a new option to protect themselves from COVID: Earlier this year the FDA approved an intravenous treatment called pemivibart, which can be given every three months. The medicine is an artificial antibody that is meant to generate an immune reaction to a COVID infection.
Treatment Remains an Option
People who catch COVID and develop serious symptoms can and should receive treatment.
“The most proven treatment now remains Paxlovid, which we still recommend for those at highest risk,” says Jonathan Li, a virologist at the Brigham and Women’s Hospital and Harvard Medical School. Paxlovid’s standard dosage is 30 pills of two antiviral medications taken over five days.
Paxlovid can interact with other medications, however, and additional COVID treatments are available. Remdesivir, currently available only as a daily injection at medical facilities, remains a valuable tool, says H. Clifford Lane, an infectious disease specialist at the National Institute of Allergy and Infectious Diseases, as does molnupiravir, another multidose, multiday oral medication.
Lane says that while these options are all clearly safe, circumstances have changed significantly from when they were first tested and approved. “The host population has changed; the virus has changed,” Lane says. Doctors don’t have the data to determine whether these medications are still making a difference in people who are at lower risk of severe disease. “It’s just not so clear if [they’re effective if] you’re an otherwise healthy 30-year-old with a runny nose, and you test positive,” Lane says. “I think most [clinicians] would not prescribe them in that setting.”