Summers are undoubtedly getting hotter. Extreme heat events are predicted to become longer, more intense and more frequent in the coming years—and rising temperatures are already taking a toll on the human body. A published last month by the U.S. Centers for Disease Control and Prevention found that heat-related emergency room visits were substantially higher from May to September 2023 than in any year before. And now growing evidence suggests that people who rely on certain medications, notably including antipsychotics, may become especially vulnerable to heat-related illness and adverse side effects as temperatures climb.
Studies have established that people with chronic illnesses such as schizophrenia, diabetes and cardiovascular or respiratory disease are generally more vulnerable to overheating—and the medications they need may actually worsen these risks. A 2020 PLOS ONE study found that various commonly prescribed drugs interfere with the body’s ability to perceive and protect itself from heat, increasing the risk of hospitalization. These include diuretics, antipsychotics, beta-blockers, stimulants, antihypertensives and anticholinergic medications (which include Parkinson’s and bladder-control medications). Illicit use of amphetamines and some other drugs, including unlicensed weight-loss drugs such as dinitrophenol, can alter body temperature.
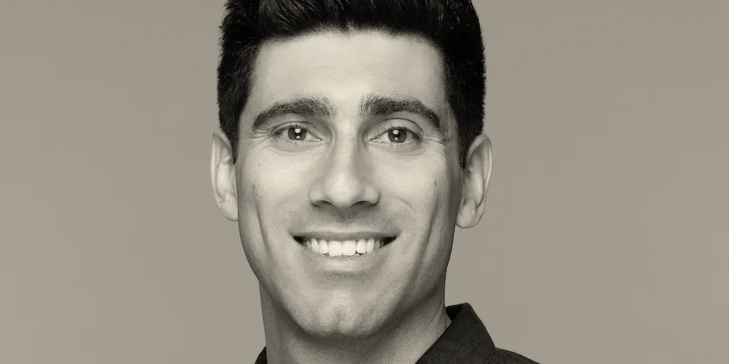
“There are a lot of drugs out there that diminish our ability to radiate off heat and cool down,” says Adam Blumenberg, an assistant professor of emergency medicine at Columbia University Medical Center. Emergency room visits for medication-related heat stress or illness, also known as drug-induced hyperthermia, are still relatively rare—but Blumenberg says this will likely change as heat waves and record-breaking temperatures continue to increase.
On supporting science journalism
If you’re enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
The human body’s built-in “thermostat” system works to maintain an internal temperature between 97 and 99 degrees Fahrenheit (36 and 37 degrees Celsius), Blumenberg says, adding that a body temperature of more than 104 degrees F (40 degrees C) can be life-threatening. The brain structure called the hypothalamus helps orchestrate processes to keep that core temperature stable when the weather gets too hot. It acts on the autonomic nervous system, which is responsible for keeping the body in homeostasis via many important processes, including heart rate, blood pressure and respiration. The hypothalamus also regulates sweating and dilates blood vessels in the skin, arms, feet and face to dissipate body heat—and it can cause a sensation of discomfort that prompts the body to seek out shade, water or rest.
Experts say many medications associated with drug-induced hyperthermia have one factor in common: they’re anticholinergic. These drugs block cells’ receptors from binding to a neurotransmitter called acetylcholine, which plays an important role in the autonomic nervous system and its heat-adjustment responses, such as perspiration. Blocking its action can cause dry mouth and urinary retention—feeling a need to urinate but being unable to do so. “Some of these medications might cause more heat sensitivity because you’re not sweating,” says Vicki Ellingrod, dean of the University of Michigan College of Pharmacy. “Your body is not making the secretions that it should be making.” Anticholinergics can also causeflushed skin, dilated pupils, blurred vision, fever and an altered mental state. Clinicians have historically used a mnemonic about these symptoms to diagnose anticholinergic poisoning.
“A lot of drugs have mild anticholinergic properties, even if that’s not their main intent as a drug,” Blumenberg says. For example, some allergy medications primarily block a cell’s histamine receptors—but they might also bind to other receptors as well and thus still produce anticholinergic effects.
Some antipsychotics and neuroleptics (first-generation antipsychotics) can also lead to this and can create a dopamine-blocking effect as well. Dopamine—often called the “feel-good” hormone—influences motivation, memory and even body movement; blocking it can make people feel stiff and cause problems with gait, balance and muscles. One way to decrease those side effects is by pairing an antipsychotic with an anticholinergic—further interfering with acetylcholine and potentially disrupting heat regulation. People who take the antipsychotic drug haloperidol for schizophrenia, for example, are often prescribed an anticholinergic drug called benztropine that decreases some adverse side effects but can, on rare occasions, elevate internal temperature. This shouldn’t happen if people take the appropriate prescribed dose, Blumenberg says, “but it’s possible.”
Antipsychotic medications, as well as medications commonly prescribed for bipolar disorder, depression and insomnia, typically act on the brain, which means they could potentially influence the neural pathways that control temperature. Some older antipsychotics are known to occasionally cause a severe reaction called neuroleptic malignant syndrome, which impacts the body’s ability to thermoregulate, Ellingrod notes. “Now, with our newer medications, it’s not as common. But maybe with the impact of the climate, it’s going to be more common,” she says.
New research into psychiatric disorders has rapidly improved existing treatments and led to new strategies to reduce some of the adverse side effects; such steps include pairing antipsychotics with other medications. But responses to medications can still vary from person to person. Additionally, “the degree in which [these drugs] actually block the acetylcholine receptors varies between medications, which is why you can see one drug in a class really having this [anticholinergic] effect and another drug in the same class not having the same effect,” Ellingrod says. For example, she adds, the antihistamines that cause more drowsiness tend to be more anticholinergic because they can cross the blood-brain barrier. Newer antihistamines have side effects that are less sedating and very rarely disrupt thermoregulation.
A 2023 study in the European Journal of Clinical Pharmacology found that most heat-related adverse effects were reported for medications that act on the nervous system (such as drugs that have strong anticholinergic effects), followed by medications that modulate the immune system. People on heart medications might face thermoregulation complications under high environmental temperatures, too. A 2022 study in Nature Cardiovascular Researchfound that people taking beta-blockers and antiplatelet medications for cardiovascular conditions have a higher risk of experiencing a heart attack in hot weather.
“Beta-receptor blockers could decrease the heart rate [and] reduce the blood flow to the skin. That makes people more vulnerable to heat exposure,” says Kai Chen, an assistant professor at the Yale School of Public Health and a co-author of the 2022 study. “The same goes for the [antiplatelet drugs], like aspirin. People taking that could increase core body temperature during passive heat stress, which will make them more vulnerable.”
Chen notes that his study is based only on a small group of German participants. But he and his team are conducting studies to analyze these effects in bigger cohorts in the U.S., and they expect results in a couple of years. “We’re trying to see if this enhanced heat effect on these certain medications is due to the medication itself or due to the preexisting conditions,” he says. “If we can confirm through multiple studies at multiple locations with different populations that this is not a mere correlation or association and can maybe indicate a causation, then I think that will change how physicians advise the patients taking the medication during heat waves.”
Soko Setoguchi, a professor of medicine and epidemiology at Rutgers Robert Wood Johnson Medical School and a co-author of the 2020 PLOS ONE study, says there is a growing effort to understand how drugs are affected by extreme heat—because any medication can have unintended effects, and there is still “limited evidence” on how heat influences various drug interactions.
“The precise temperature threshold for these side effects to occur is not explicitly defined in the provided studies, as heat sensitivity can vary based on individual health status, medication dosage and specific environmental conditions,” Setoguchi says, adding that comprehensive data from larger trials are needed.
The Food and Drug Administration monitors drugs’ safety even after they are approved, but it has not been tracking heat-related issues associated with medications. “If newly identified safety signals are identified,” the agency wrote in an e-mail to Scientific American, “the FDA will determine what, if any, actions are appropriate after a thorough review of available data.”
Scientific American requested comment from 10 major pharmaceutical companies that make antipsychotic medications, but only one, Lundbeck, had responded by the time of publication. A spokesperson said in an e-mail that the company hasn’t “observed any side effects linked to weather conditions such as hot weather in relation to the use of antipsychotics. However, certain labels may mention side effects like flushing, tremor, and hyperthermia, which are linked to [medications that act on serotonin] and can resemble symptoms associated with hot weather.” (Serotonin is a hormone involved in temperature regulation.)
Ultimately, some medications that can induce heat-related side effects are still necessary for treating certain conditions. Experts recommend consulting with physicians about potentially adjusting doses or scheduling and alerting a health care provider if any irregular reactions occur as the weather warms. Additionally, people taking medications known to produce an anticholinergic effect should be aware of strategies to keep cool. These can include staying hydrated, carrying fans or ice packs and seeking shade or air-conditioning. Until more research results emerge, clinicians and their patients should discuss best options for prescriptions—and ways to prepare for hotter days.