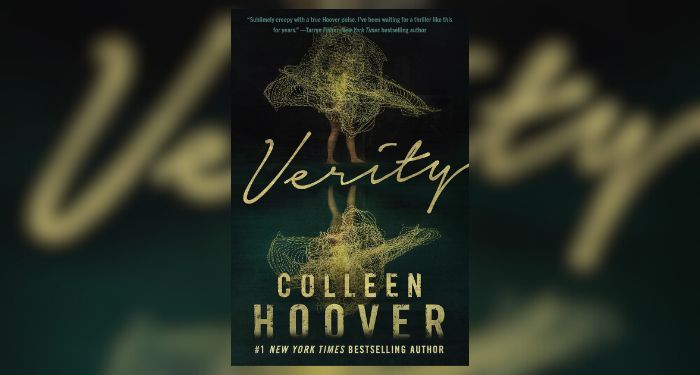
Tirzepatide is sold under the name Mounjaro to treat type 2 diabetes
Shutterstock / Mohammed_Al_Ali
A weight-loss drug called tirzepatide has received approval from the US Food and Drug Administration (FDA) for adults who are overweight or have obesity and at least one weight-related condition, such as high blood pressure or type 2 diabetes. In clinical trials, it reduced body weight by an average of almost 21 per cent in people who were overweight or had obesity.
“That’s the most weight loss we’ve ever seen with a medication,” says Louis Aronne at Weill Cornell Medicine in New York. “[It is] a magnitude of weight loss that’s equivalent to surgery.”
The prescription medication, developed by US pharmaceutical company Lilly, was previously approved under the name Mounjaro for treating type 2 diabetes. It is now the seventh medication approved for weight loss in the US.
“With rising rates of obesity, there’s been an increased demand for medications indicated for weight management, and we have faced shortages in the past,” says Priya Jaisinghani at NYU Langone Health in New York. Tirzepatide’s approval will increase supply and hopefully reduce these medication shortages, she says.
Tirzepatide, sold under the brand name Zepbound, is a once-weekly injection that mimics two hormones: GLP-1 and GIP. The body naturally produces GIP once we start eating, which increases hunger, and then releases GLP-1 after eating to trigger the sensation of fullness, says Aronne. “For reasons we still don’t understand, when you give [GIP] along with GLP-1, it reduces appetite even further,” he says.
The combination is probably why tirzepatide is so effective. In a clinical trial published in 2022 by Aronne and his colleagues, more than 2500 adults with obesity, but not diabetes, took either a placebo or a low, medium or high dose of tirzepatide for 72 weeks. People given the highest dose lost, on average, nearly 21 per cent of their body weight, or almost 24 kilograms. Meanwhile, those on the lowest dose lost 15 per cent of their body weight, or about 16 kilograms. By comparison, the popular weight loss medication semaglutide – which mimics GLP-1 – reduces weight by an average of about 15 per cent, though a trial directly comparing the two hasn’t been completed.
Tirzepatide also reduced cholesterol levels, insulin and blood pressure in people on the medication, and improved their physical mobility. “Once you get to 15 per cent or greater weight loss, which is the majority of people taking a medicine like this, most of the complications that we associate with obesity will improve,” says Aronne.
Tirzepatide does come with side effects, however, including nausea, constipation, diarrhoea and vomiting. People on tirzepatide can also regain lost weight once they stop using the medication – a common caveat of most weight loss medications.
This is concerning given that the long-term health risks of tirzepatide are unknown. Medications mimicking only GLP-1, like semaglutide, have been around for several years. Some evidence suggests they may increase the risk of certain cancers, kidney conditions and serious gastrointestinal problems, but incidences are rare. Tirzepatide has been shown to cause thyroid tumours in rats, though it is unclear if it does so in humans, according to the FDA. As such, the agency says people with a personal or family history of medullary thyroid cancer and those with certain inherited endocrine disorders should not use the medication.
For many people with obesity, the health benefits of tirzepatide outweigh its potential downsides. “One of the best outcomes can be reversing complications that are associated with [overweight and obesity],” says Jaisinghani. “By reversing some of those complications we now have an opportunity to potentially take people off other medications, and this not only improves their health, but their quality of life.”
Topics: