Two drugs called dexamethasone and diclofenac relieve back pain in the short term, but may block healing of the injury and so cause worse pain long term
Health
11 May 2022
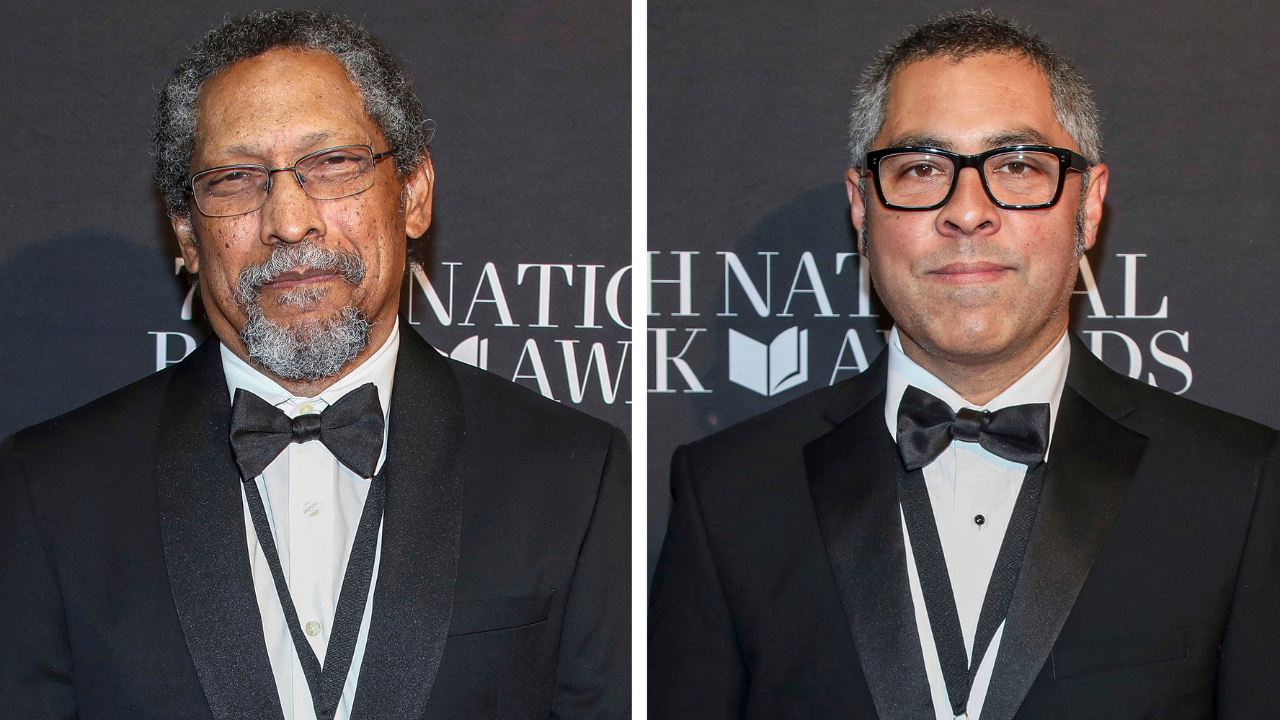
Some drugs used to treat back pain might make things worse Shutterstock / Cavan Images – Offset
Two anti-inflammatory drugs commonly used for back pain may be inadvertently making the condition worse.
The medicines, called dexamethasone and diclofenac, may interfere with the body’s normal processes for healing the injured tissue, early-stage research suggests. But the idea hasn’t yet been tested in a randomised trial, the best kind of medical evidence.
Lower back pain is one of the most common conditions worldwide, with about four in five people experiencing it at some point, but the causes are often unclear.
Some of those affected are shown in scans to have an outward bulge in one of the discs in the spine that cushion the vertebrae – known as a slipped disc – but many people without back pain have such a bulge too.
As opioid painkillers can be addictive, doctors may prescribe anti-inflammatory medicines instead. This is because pain can be worsened by inflammation, which is a low-grade activation of immune cells.
Luda Diatchenko at McGill University in Montreal and her colleagues investigated 98 people who had recently developed lower back pain. The researchers took regular blood samples and analysed them to see which genes were active in the immune cells circulating in the blood.
In those whose pain subsided over the next three months, one type of inflammatory immune cell – the neutrophils – showed higher levels of activity than in people whose pain persisted. This suggests that some inflammatory cells can help people overcome their pain – a process that might be disrupted by anti-inflammatory drugs.
Diatchenko’s team also found that in mice given a back injury, treatment with anti-inflammatories such as dexamethasone and diclofenac relieved their pain in the short term, but led to more pain longer term. Without any anti-inflammatory drug treatment, the animals also experienced longer-term pain if their neutrophils were killed by injections of an antibody.
“Inflammation is painful, but this inflammation is needed for our body to resolve pain,” says Diatchenko. “Pain resolution is an active process that requires neutrophil activation.”
Next, the team looked at people who had filled out surveys as part of a long-running medical study called the UK Biobank. Those who had reported new back pain were more likely to see their problem persist if they were taking non-steroidal anti-inflammatory drugs such as diclofenac than if they were taking other painkillers such as paracetamol.
A problem with this part of the study is that people who had worse pain could have been more likely to be prescribed an anti-inflammatory, says Diatchenko – meaning that the drugs don’t cause prolonged pain, they merely correlate with it.
As the UK Biobank study didn’t ask people about their pain severity, the team instead adjusted these results by taking into account how many different sites of pain each person had, which previous work suggests correlates with pain intensity. “But that is only a proxy,” says Gene Feder, a doctor in Bristol, UK, who specialises in treating back pain.
To really see if anti-inflammatory medicines make back pain persist, we would need a randomised trial comparing different kinds of painkillers, says Feder. “For me to change my prescribing behaviour I would really want to see a human trial. This leaves me with a lot of uncertainty.”
Journal reference: Science Translational Medicine, DOI: 10.1126/scitranslmed.abj9954
Sign up to our free Health Check newsletter that gives you the health, diet and fitness news you can trust, every Saturday
More on these topics: