Whenever social risk factors arise, “there’s an opportunity for someone to fall through the cracks or experience a delay,” says Phillips, who is now a data scientist at Georgia State University (she was not involved in the research). That delay could take many forms, “whether it’s cancer not diagnosed as early as it should have, receiving treatment, missing appointments, and not getting treatment in the way they should have,” she says.
But whether housing insecurity specifically is responsible for increasing cancer mortality isn’t yet proven. The issue of housing might simply be “mimicking other factors,” argues Stuart Butler, a senior fellow in economic studies at the Brookings Institution. An insecure living situation could just be another indicator of financial insecurity, which itself has negative health impacts. Social risks “rarely stand alone,” says Banegas, the study lead. “It’s rare that someone only has housing instability. The picture is more complex.”
Even if the exact nature of the link isn’t clear, the connection between housing and health suggests that improving people’s living security would have compound benefits. But it’s a big issue to address. In the US, some programs exist for supporting people with housing, but they are limited in the amount of support they can provide and who qualifies for benefits, leaving enormous gaps in affordable housing for many people.
The question then is: “Who is best available to invest?” says Butler. Whether it’s a manager in a housing agency or the leadership of a hospital, investing in housing—or measures to address social deprivation more generally—often won’t be seen as an integral part of their business’s model. The US health system—including people who provide cancer care—does what it can, but social risks are broad problems that require policy and funding to remedy them. There’s no “magic bullet” for getting the scale of investment needed to tackle something like housing insecurity, Butler says.
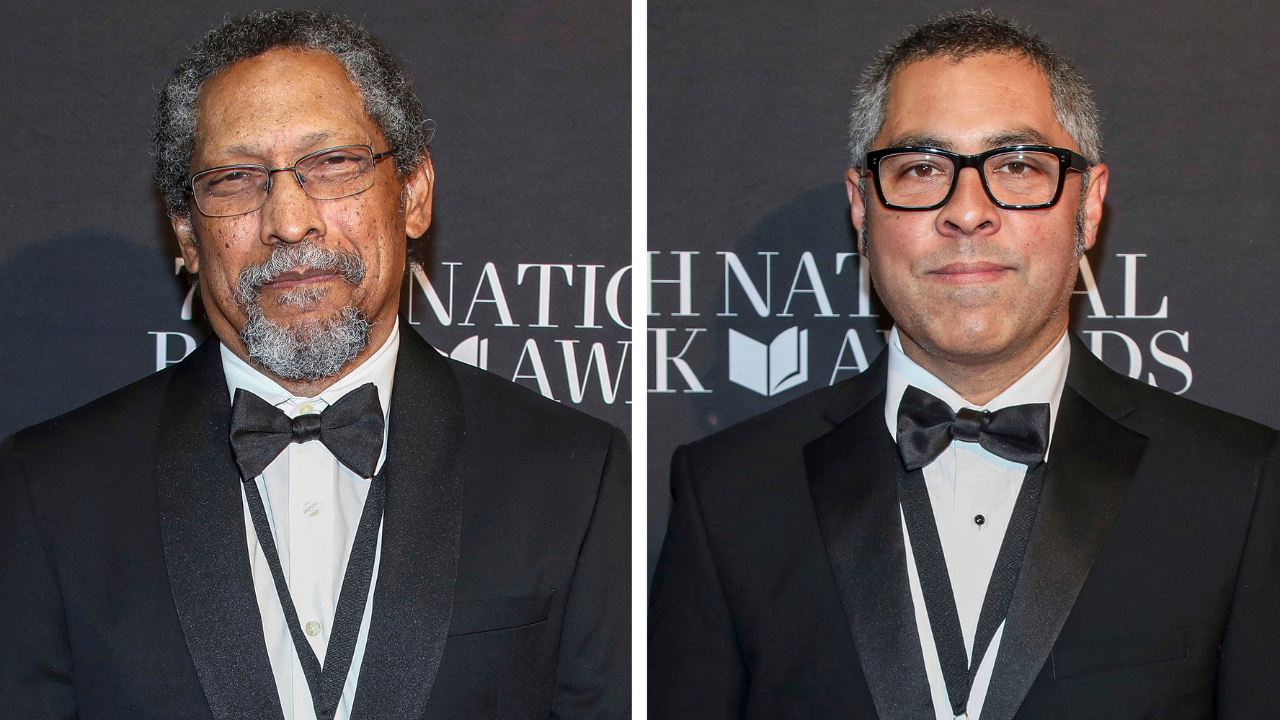
A further dimension is that some groups are more likely to suffer from housing insecurity—potentially putting them at greater risk from cancer. Research published in 2019 showed that in parts of the US where Black populations suffer mortgage discrimination—that is, where lenders discriminate against customers based on race—the disparity in cancer mortality between Black and white people is also larger. Groups that disproportionately experience housing insecurity are more likely to be those “that have historically been marginalized and have less financial resources to weather their cancer and receive treatment,” says Pollack.
So it’s not one factor alone that likely contributes to cancer disparities, but rather the joint impact of race, ethnicity, housing, and other different factors acting together, argues Biplab Datta, assistant professor at the Institute of Public and Preventive Health at Augusta University. A potential solution is identifying populations that are at greater risk from cancer, he says, and if housing insecurity is higher among a population or location, then critical improvements—such as improving cancer screening and quality of care, and reducing stress—should be pursued in those places, through policy.
In New York City, the patient that Phillips saw was fortunate to receive timely cancer care, despite her obstacles and social risks. But this isn’t the case with every patient—and that will remain the case while housing insecurity remains widespread.