After completing six long rounds of chemotherapy, 75-year-old Pedro R. L. received the news he and his family had been hoping for: his chronic lymphocytic leukemia was in complete remission. But while his body was still recovering, he contracted COVID-19. He was admitted to the Quirónsalud Madrid University Hospital on January 30, 2021. Initial treatments failed, and by February 25 he had developed severe pneumonia. That’s when his doctor, Pablo Guisado, recommended they try plitidepsin, a potent antiviral compound in a phase 3 clinical trial for treating hospitalized COVID patients.
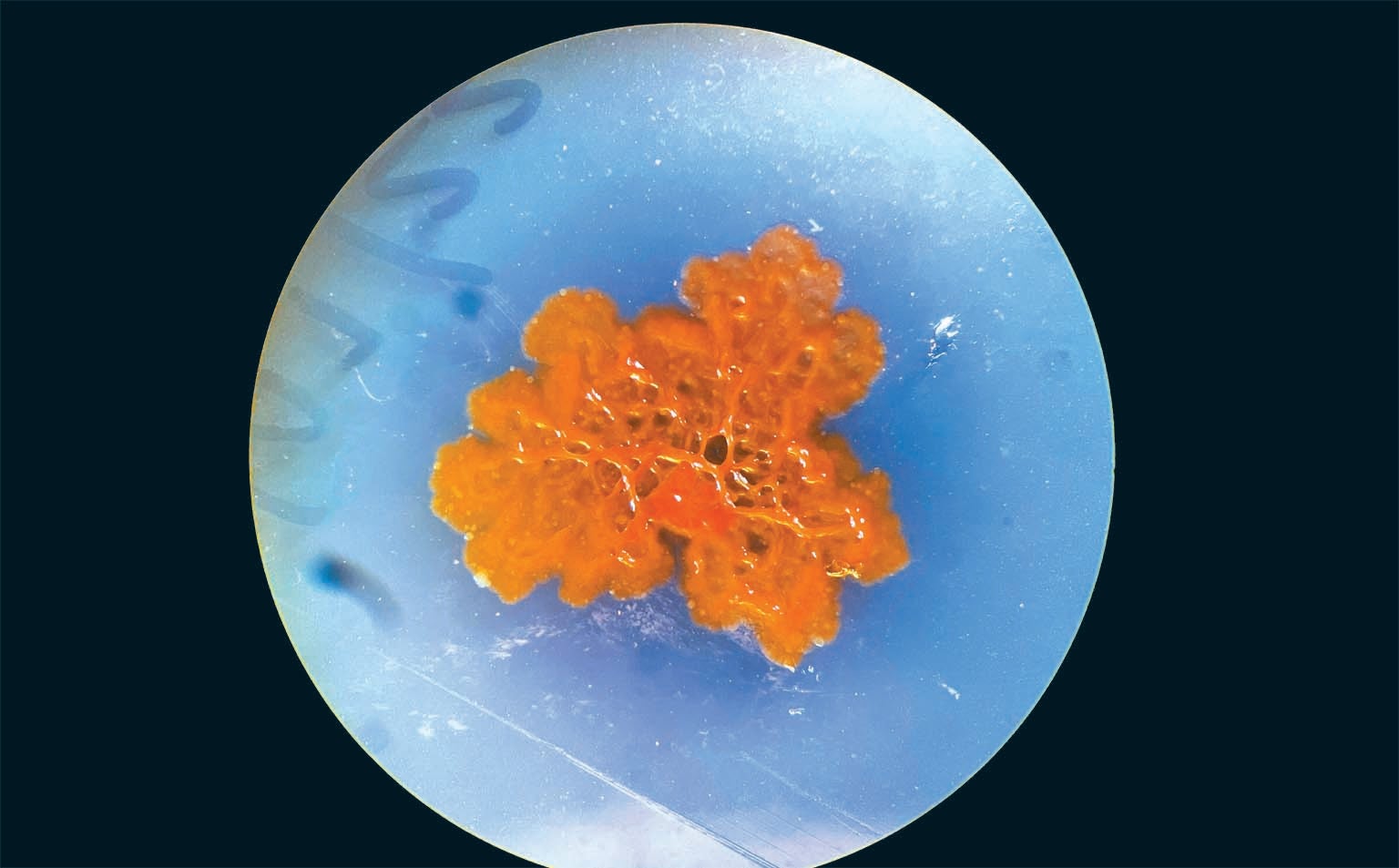
Plitidepsin comes from a place few drugmakers would have predicted: the seafloor around Es Vedrá, an uninhabited rocky island off the southwestern coast of Ibiza, Spain. Back in 1988, Madrid-based pharmaceutical company PharmaMar organized an expedition to the storied site, an abrupt outcrop thought to have inspired Homer’s tale in The Odyssey about singing sirens luring sailors to their death. While diving on a reef packed with purple corals and red sea fans, scientists pulled a comparatively uninspiring invertebrate creature from a rocky slope 36 meters deep—a translucent, pale-yellow tunicate, Aplidium albicans, that resembled a wad of discarded facial tissues.
The researchers were interested in tunicates because they filter-feed on plankton by continuously drawing water through their barrel-shaped bodies. Along with their food, they pull in viruses and other pathogens, so they need strong chemical defenses to fight off infectious organisms—and that makes them promising sources for medicines.
By 1990 PharmaMar had isolated a compound from the A. albicans specimen that was active against both cancer and virus cultures. PharmaMar pursued the cancer angle because cancer drugs tend to be more profitable than antivirals. After decades of research and testing, in 2018 Australia approved plitidepsin as a treatment for multiple myeloma.
When the COVID pandemic hit, company scientists quickly proved that plitidepsin was effective against SARS-CoV-2 in both laboratory cultures and mice, and it outperformed competing antivirals in preclinical, head-to-head trials. In 2020 PharmaMar launched a phase 1-2 clinical trial for hospitalized COVID patients that concluded in 2021. The results were dramatic: 74 percent of the patients with moderate disease recovered fully within a week of their first dose. The phase 3 trial is due to finish by December. In May, PharmaMar virologist Jose Jimeno said plitidepsin appeared to be superior to other COVID antivirals. Its impact on Pedro R. L. was impressive; after two courses of treatment, his pneumonia and the rest of his symptoms had cleared completely.

Today, worldwide, there are 21 approved drugs that were sourced from the sea, most of them isolated from invertebrates. Another tunicate, Ecteinascidia turbinata, which attaches to submerged mangrove roots, yielded the molecular mixture that led to Yondelis, a sarcoma and ovarian cancer drug, and Zepzelca, which targets small-cell lung cancer. A black sponge that encrusts tidal pool rocks in southern Japan, Halichondria okadai, produced a drug, now marketed as Halaven, to treat late-stage breast cancer. And a venom peptide from a cone snail, Conus magus, led to Prialt, a chronic pain drug.
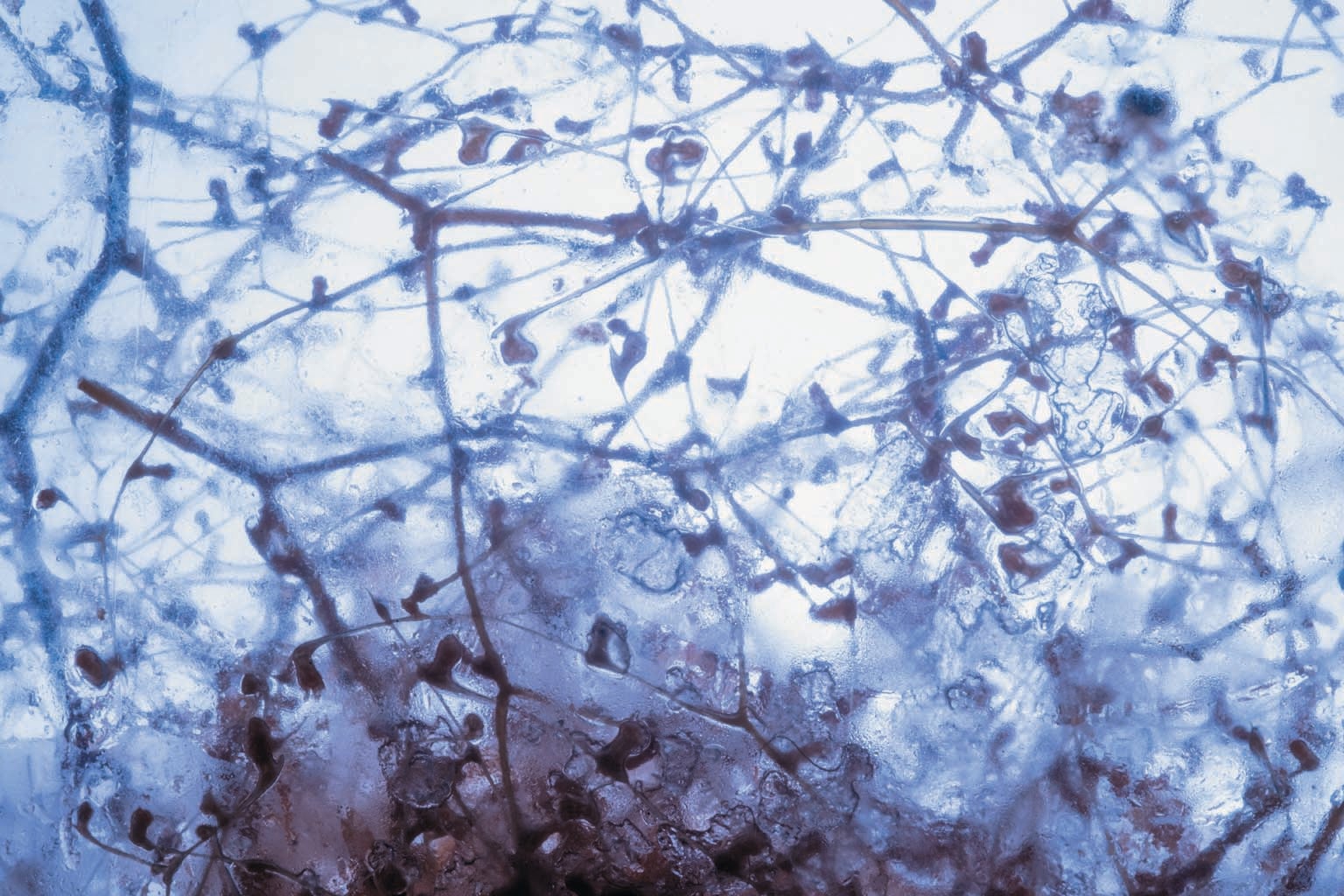
Corals, sea slugs, marine worms and mollusks have also yielded promising compounds. “For the past 600 million years these invertebrates have been living in this microbial soup that’s like a petri dish,” says marine ecologist Drew Harvell of Cornell University, explaining their need for robust defenses. An average liter of seawater contains about one billion bacteria and 10 billion viruses. Although scientists first assumed most marine invertebrates evolved their own weapons, they have learned over the past few decades that the majority of these defensive substances are actually produced by microbes living symbiotically within the creatures’ tissues. Last year, for instance, a team led by Samar Abdelrahman of the Georgia Institute of Technology tested five species of sea slugs from the Red Sea and found bacteria that produced antibacterial, antifungal and anticancer agents.
Drug discovery scientists—who for decades focused on land-based biology because it was more familiar and easier to access—now widely recognize that microbes, which dominate the ocean’s biological diversity, are the most likely sources of marine-derived medicines. Of 23 new drugs currently in clinical trials, 16 are produced by microbes, and another four come from invertebrates that probably owe their resilience to symbiotic microbes. In recent years scientists have isolated thousands of promising compounds from marine microbes, the diversity of which reflects the vast variability of marine conditions. “On land, microbes dry out; they have trouble maintaining a fluid balance,” Harvell says. “But the oceans are a much more permissive, welcoming environment.”
Yet for most approved marine drugs, the process has taken decades, partly because of insufficient funding and partly because isolating, testing and producing large quantities of novel compounds is time-consuming. Fortunately, recent advances in genomics, chemistry and computation are enabling scientists to be more targeted and efficient in the search for lifesaving medicines from the sea.
Gene Targets
In 1989 Paul Jensen brought sediments from the Bahamian seafloor back to his lab at the Scripps Institution of Oceanography to mine them for medically useful bacteria. It wasn’t easy. His first challenge was to grow marine bacteria in lab conditions that are, at best, an approximation of those in the ocean. Then, when some species grew, he had to persuade them to produce at least a few of the molecules in their arsenal, even though they weren’t subject to the same stimuli they would face in their natural environment.
Despite these hurdles, Jensen eventually discovered a new species of bacteria, Salinispora tropica, that produced a novel cancer-killing molecule. That compound, now marketed as marizomib, has just completed a phase 3 trial as a drug for glioblastoma, the deadly brain cancer that claimed the lives of John McCain and Beau Biden. It is currently awaiting approval from the Food and Drug Administration. Marizomib is a powerful example of the potential for marine bacteria to yield new medicines, but the process took more than three decades, motivating Jensen and others to look for better approaches.
By the early 2000s genomics had transformed their work. The first full genome sequences for marine microbes, including S. tropica, revealed that species that produced just a few compounds in lab cultures could usually make many more; some of them had dozens of compound-encoding gene clusters in their DNA. Within a few years metagenomics—the process of sequencing the DNA of entire communities of organisms in a sample—revealed still more hidden potential. Scientists started to find compound-encoding gene clusters in species they hadn’t even cultured in the lab.
Today Jensen is also looking directly for molecules instead of the microbes that produce them. On four occasions over the past year, postdoctoral researchers on his team have waded into the seagrass beds off San Diego’s Point Loma peninsula to submerge sheets of tiny, absorbent beads, called resins, that pull organic molecules out of seawater. Back in the lab, Jensen analyzes the samples for bioactive compounds—chemicals that can act on a living organism.

He already has a hit: a compound with an unusual carbon skeleton that includes a group of enzyme-reactive molecules Jensen thinks could act “as something like a warhead.” This novel structure might function very differently than existing medicines do. “I think it’s going to kill cells,” Jensen predicts. “Now we’re hoping to get a sense of what its target might be.”
Next, he will need to match the compound to its producer. Enormous databases of marine microbial genomes and bioactive compounds, along with the computing power necessary to correlate them, are enabling scientists to link chemicals to genes efficiently. Katherine Duncan, a marine microbial chemist at the University of Strathclyde in Glasgow, is a pioneer of this approach, which she calls pattern-based genome mining. The technique has become possible only recently. “We just haven’t had the tools to compare data sets of this size,” she says.
Duncan is now using this technique to analyze dark sediment cores pulled from the ocean floor 4,000 to 4,500 meters deep off the coast of Antarctica. The early results are tantalizing: The samples include at least two new species of marine bacteria, Pseudonocardia abyssalis and Pseudonocardia oceani, that produce antimicrobial compounds. On land, members of the same genus live symbiotically with fungus-growing ants, producing antibacterial and antifungal molecules that deter pathogens from invading the ants’ fungal gardens. It’s not a stretch to imagine that the marine cousins could yield anti-infective drugs.
One of the greatest challenges scientists such as Duncan and Jensen face is figuring out which molecular discoveries warrant the most attention. Nadine Ziemert, a microbiologist at the University of Tübingen in Germany, has developed a tool to help researchers mine genomes in a more targeted way by looking for resistance genes. Any organism that produces a toxic molecule must have some mechanism for protecting itself from its own weapon—usually by making a modified copy of the toxin’s cellular target that can resist its attack.
Ziemert’s tool, called the Antibiotic Resistant Target Seeker, allows researchers to access a database of more than 10,000 bacterial genomes—or upload their own—and run a search for resistance genes related to specific cell functions. The database will become more valuable as it grows, especially as researchers accelerate their work to sequence the genomes of species from extreme, underexplored environments. Ziemert’s target seeker has shown such promise that start-up company Hexagon Bio has built a similar tool to mine fungus genomes for promising compounds.
New Antibiotics
Targeted genome mining couldn’t come at a better time. The COVID pandemic has highlighted the need for a deeper pool of drugs to treat emerging infectious diseases. There is also a desperate need for new drugs to treat established diseases. Many bacterial infections, including pneumonia, tuberculosis, gonorrhea, blood poisoning and various foodborne diseases, have become harder—and in some cases, impossible—to treat because of rising microbial resistance to antibiotics. Public health officials widely recognize antibiotic resistance as one of the gravest threats facing humanity.
Because almost all antibiotics come from terrestrial microbes, it seems clear that marine microbes, which are greatly understudied, hold the potential to address this crisis. University of Sydney chemist Richard Payne is particularly excited about their ability to treat tuberculosis, caused by Mycobacterium tuberculosis. “Over the last 10 years TB has been the greatest killer among infectious diseases,” Payne says, “and with all the efforts that have gone to COVID, we’ve gone backward with our control of TB.” An antibiotic that targets a different TB protein than past drugs is needed.
That’s exactly what Payne found in a bacterium from Shinyang Beach on Jeju Island, South Korea, a horseshoe of white sand on a small peninsula best known for its ideal windsurfing and kitesurfing conditions. The compound, ohmyungsamycin A, prevents M. tuberculosis from properly disposing of its waste proteins, ultimately killing the cell. And when Payne created a set of chemical analogs—slightly altered, chemically synthesized molecules that could be produced in volume—one of them was so potent that it completely sterilized a lab-grown tuberculosis colony in three days. The drug has already proved effective in infected zebra fish and is moving on to trials in mice.
Finding and developing new antibiotics have largely fallen to academics in recent decades because the drugs sell at such low prices that pharmaceutical companies lack the financial incentive to pursue them. The same math applies to treatments for many neglected tropical diseases, including malaria. In 2012 Scripps chemist William Gerwick isolated a molecule called carmaphycin B from a tuft of cyanobacteria growing on a boat’s mooring line in a Curaçao harbor. He chemically synthesized a set of analogs that he tested against cancer cells, a frequent first line of research.
The results were not spectacular, so Gerwick turned his attention to other projects. Recently, however, a colleague suggested that they test his analogs on malaria parasites, and this time the outcome was striking. “One of them was exquisitely reactive against malaria,” Gerwick says. Moreover, it wasn’t toxic to human cells.
Gerwick now has funding to explore carmaphycin B as a new antimalarial drug. Whether or not it eventually becomes an approved medicine, the discovery is a reminder about the possibilities stored in the thousands of bioactive marine compounds scientists have already identified.
Carmaphycin B is also a reminder that technological advances alone won’t deliver new drugs; serendipity and a willingness to capitalize on it are often required. On the day that Gerwick’s former student Joshawna Nunnery collected the cyanobacteria from the mooring line, she was supposed to be diving elsewhere. But when her lab mate and diving partner contracted dengue fever, she had to cancel those plans and resorted to snorkeling near the research station instead.
Opportunities to capitalize on such serendipity are increasing as investment in ocean exploration grows. On a recent expedition to the central Pacific Ocean’s Phoenix Islands archipelago onboard the Schmidt Ocean Institute’s research vessel, Falkor, Anna Gauthier became one of the first scientists to sample deep-sea bacteria from the islands. Gauthier, a doctoral student at Harvard University, planned to conduct immune response experiments during the expedition, so she didn’t immediately freeze bacteria she pulled from the sea, which is the usual practice. Instead she started culturing the organisms onboard the ship.
The technique provided an unintended benefit: survivorship was far higher than in traditional, lab-based cultures of defrosted specimens. Eighty percent of the bacteria she grew were so different from those typically encountered by mammals that they didn’t trigger an immune response from mammalian cells. The finding, though still far from leading to a medical advance, has tantalizing potential for immunotherapies and vaccines.
The promise of new lifesaving medicines, paired with rising public health crises, offers tremendous motivation for scientists such as Duncan in Glasgow. “I know people who have been on last-line antibiotics and were resistant,” she says. “My grandma died from sepsis. Everyone has stories like that.”
Duncan hopes those stories may change within the next decade. “The marine environment is hugely undiscovered,” she marvels. The next plitidepsin is out there in the ocean. It might already be in a lab.































![‘911 Lone Star’ Season 5 Episode 8: Tommy’s Cancer Setback [VIDEO] ‘911 Lone Star’ Season 5 Episode 8: Tommy’s Cancer Setback [VIDEO]](https://tvline.com/wp-content/uploads/2024/11/911-lone-star-season-5-episode-8-tommy-cancer.jpg?w=650)