A review of 17 previous studies finds no evidence for a link between depression and low serotonin levels, which SSRI antidepressants focus on – though not everyone is convinced by the findings
Health
20 July 2022
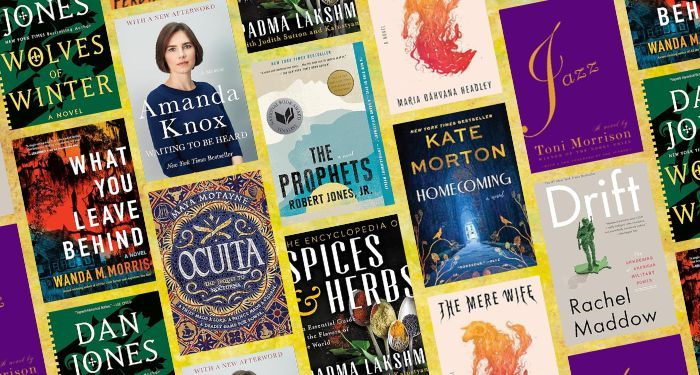
Polarised light micrograph of crystals of serotonin, which is a neurotransmitter in the brain MICHAEL W. DAVIDSON/SCIENCE PHOTO LIBRARY
There may be no link between serotonin levels and depression, according to an analysis of 17 studies. This raises questions about antidepressants that focus on this brain-signalling molecule, say the authors of the analysis. Not everyone is convinced by the findings, though.
The serotonin hypothesis, which dates from the 1960s, says that a chemical imbalance in the brain, including low levels of serotonin, also known as 5-hydroxytryptamine or 5-HT, leads to depression. We now think various biological, psychological and environmental factors play a role, but the most popular antidepressants, known as selective serotonin reuptake inhibitors (SSRIs), increase the availability of serotonin in the brain.
Now, Joanna Moncrieff at University College London and her colleagues have done an “umbrella analysis” of 17 systematic reviews and studies, which together included hundreds of thousands of people with and without depression.
It is difficult to directly measure real-time serotonin levels in the brain, so the 17 studies looked at depression and proxies for serotonin, such as the molecules in cerebral fluid that serotonin breaks down into; the levels of serotonin receptors and how active they are; or whether there are more genes for serotonin transporters – which remove serotonin – in people with depression.
Moncrieff’s team found that there was no evidence that low serotonin activity or amounts cause depression.
“The implication of our paper is that we do not know what [SSRI] antidepressants are doing,” says Moncrieff. One possibility is that they are working through a placebo effect, she says.
However, Johan Lundberg at the Karolinska Institute in Sweden says a limitation of the analysis is that it didn’t distinguish between people who had ongoing depression and those who have episodes of depression, whose state at the time they were assessed could affect the functioning of their serotonin systems. “It is key to separately analyse data from studies that examine the same patients when ill and when in remission, to have optimal conditions to examine the hypothesis,” he says.
Moncrieff says the review was dependent on the studies that had already been done, none of which highlighted any difference between people who were experiencing symptoms of depression or had a history of it.
“It must be recognised that 5-HT is likely only one contributor to depression,” says Paul Albert at the University of Ottawa in Canada. “Given the large placebo effect in treatment of depression, it is likely that the contribution of other systems, including dopamine that is implicated in placebo effect, may be greater than that of 5-HT.”
“Antidepressants are an effective, NICE-recommended treatment for depression that can also be prescribed for a range of physical and mental health conditions,” a spokesperson for the Royal College of Psychiatrists told the Science Media Centre in the UK, referring to treatment guidelines from the National Institute for Health and Care Excellence (NICE) in England. “Antidepressants will vary in effectiveness for different people, and the reasons for this are complex. We would not recommend for anyone to stop taking their antidepressants based on this review, and encourage anyone with concerns about their medication to contact their GP.”
Journal reference: Molecular Psychiatry, DOI: 10.1038/s41380-022-01661-0
Need a listening ear? UK Samaritans: 116123; US National Suicide Prevention Lifeline: 1 800 273 8255; hotlines in other countries.
Sign up to our free Health Check newsletter that gives you the health, diet and fitness news you can trust, every Saturday