After five years of marriage, in November 2019, my husband and I decided we were ready to try to conceive (referred to as TTC in the fertility app chat groups). A little over a year later, I finally received my first positive pregnancy test.
Due to some spotting and first-time jitters, we were able to get an early ultrasound and at around seven weeks saw a peanut-sized blob with a blinking dot, signifying a heart beat. While we knew the advice to refrain from announcing to the world, we did share the news with our parents, who shared in our joy and excitement.
At our 12-week appointment, the ultrasound technician was less talkative and there was no showing of images on the screen. Armed with just one photo, my husband and I were sent back to the lobby to wait for the doctor.
As soon as we sat down, I whispered to my husband, “Something is wrong.” After what felt like hours, but in actuality was less than 20 minutes, we found ourselves sitting in the doctor’s office as he explained to us that a heartbeat could not be located.
While we knew this was a possibility, it did not soften the blow. It had only been two months, but we’d already begun imagining our life as a family of three. I had started a private registry and researched car seats, strollers and baby monitors. We had discussed names. We had holiday cards printed and addressed, ready to be dropped in the mail announcing our new addition. Within minutes, all of those dreams were crushed. Our baby was gone.
After several blood tests to confirm the miscarriage, I was scheduled for a dilation and curettage, or D&C, at the local hospital within a week. While the experience was heartbreaking, the procedure went smoothly and after a few months of healing both physically and emotionally, we were once again trying to conceive.
In July 2021, I found myself pregnant again. Thanks to timing, I was able to tell my husband on his birthday. What a perfect gift! While we knew from our first experience that we should try to contain our excitement, it was difficult.
Our previous experience coupled with more spotting meant we were able to again get in early for an ultrasound, which yielded confirmation of a pregnancy and heartbeat. Our 12-week ultrasound also went differently, with the tech showing us the flickering dot and sending us back to the waiting room with multiple sonogram images. We breathed a collective sigh of relief as we waited for the doctor, unaware of what awaited us.
When we met with the doctor, he pulled up the sonogram on his computer and began to point out excess fluid behind the head of our fetus. He explained that this fluid was right on the cusp of irregularity and could potentially signal hydrops fetalis, a condition often caused by a chromosomal abnormality and indicative of genetic or developmental issues. He cautioned us to remain optimistic and provided us options, including additional testing and a visit to a specialist.
Within days, I had a blood draw for genetic testing (which would indicate the possibility of a chromosomal abnormality) as well as an appointment with a specialist in a large city approximately an hour from home.
The specialist performed a high-level ultrasound, which confirmed the initial findings that an abnormal amount of fluid was present in the head of the fetus. I also underwent chorionic villus sampling, an uncomfortable procedure where a small piece of the placenta is removed and sent in for chromosomal testing.
And then we waited. Fourteen days felt like years as we tried to stay optimistic and realistic at the same time. The blood test results came in and reported no abnormalities, with the chorionic villus sampling results confirming the finding. This meant I was not a carrier and we could all but rule out any chromosomal issues.
At our second appointment with the specialist, another ultrasound revealed fluid in the lungs and abdomen as well as the head. At this point, we knew our baby had a serious medical issue, but didn’t know why.
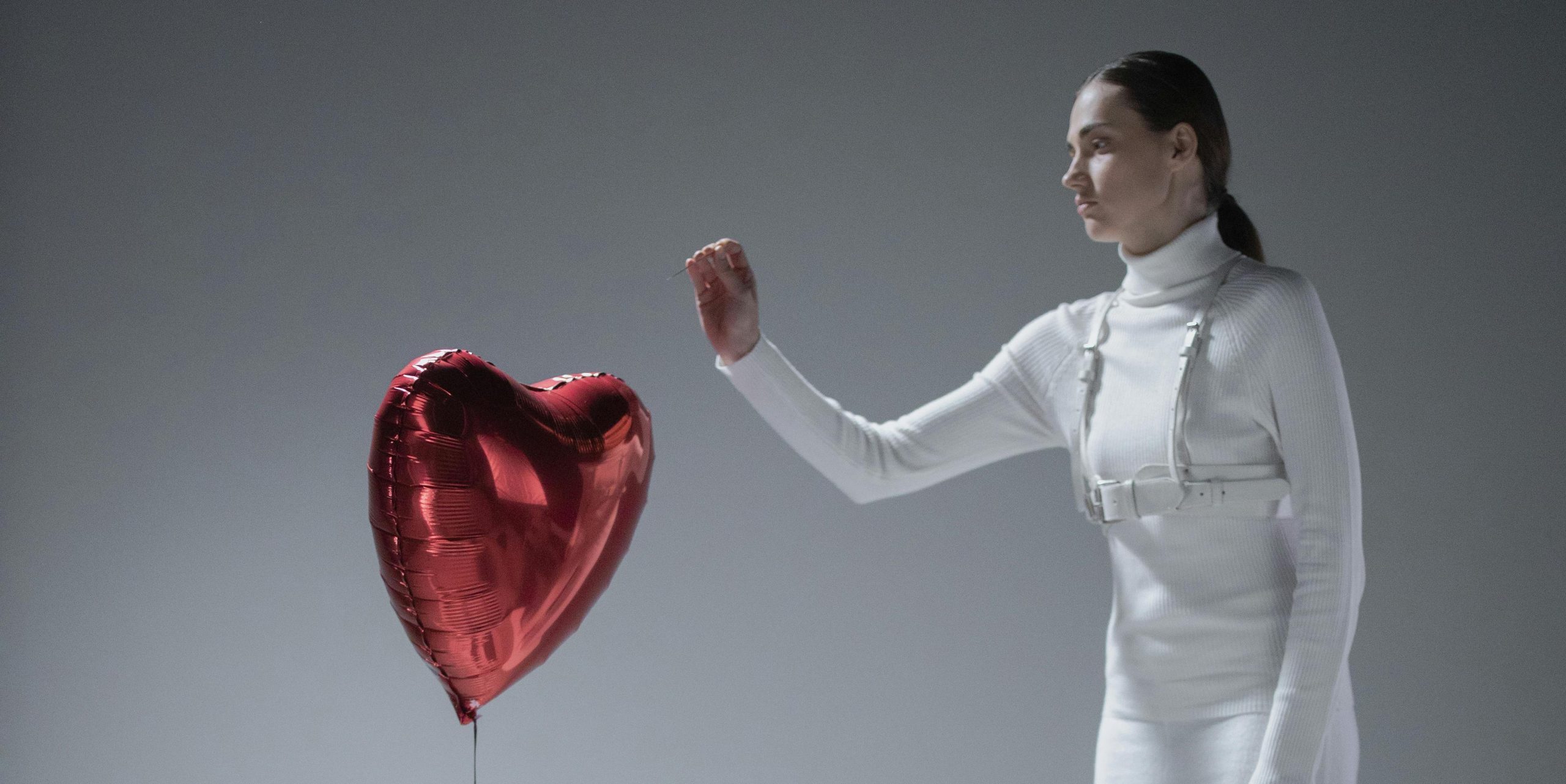
After discussions with both the specialist and my primary OB, as well as extensive independent research, my husband and I accepted the reality that the chance of our baby making it to full-term was slim. We also knew that, should we have a successful pregnancy, our child would most likely be born with a serious medical issue. Together, we decided that it would be cruel to risk bringing a child into the world that would suffer and ultimately live a short and unfulfilling life. For us, the right decision, though a hard one, was to end the pregnancy.
While I had hoped the most difficult part of this process ― making this impossible decision ― was behind us, scheduling an abortion proved challenging. Unlike my D&C, because my fetus had a heartbeat, I could not have the procedure performed by my regular OB at a local hospital.
Instead, I had to make an appointment at a medical facility that performed abortions. My doctor was incredibly supportive and helpful throughout this process and worked with me to provide a recommendation on a facility, which ended up being Planned Parenthood.
I was able to secure an appointment, but due to demand and limited availability I was forced to schedule it more than two weeks out. This meant that for two additional weeks, despite the fact I knew our fetus was not viable, I remained mentally and physically pregnant.
I continued to experience the symptoms of pregnancy and felt irresponsible making any choices that would harm my fetus, despite the fact I knew it was not viable. On one hand, I dreaded the day of my appointment, while I also looked forward to being able to move forward.
The day of my procedure required a day off work, an hour drive (thankfully with the company of my mother and husband), and a payment of $1,115. (I received a reimbursement from my insurance company, but many do not have this luxury and must face a taxing out-of-pocket cost.)
After pages of intake paperwork, an ultrasound and a conversation with a clinician, I underwent pre-surgery preparation and sat in a pre-op room for four hours. Because I was more than 16 weeks pregnant, the process was more intensive, and markedly more uncomfortable.
Once my body responded to the medications, I was brought into the operating room. While heavily medicated, I was awake during the procedure. Lying in the cold, sterile space, conscious of what was happening, I couldn’t help but second-guess my decision. This was not the experience I conjured up when I imagined having a baby. The practitioners in the room attempted to distract me and provided additional medication when I expressed discomfort, but the reality of what was happening could not be ignored.
The surgery lasted no more than 15 minutes, but it’s a memory that will be forever burned in my memory. Relief mixed with heartache as the doctor wrapped up and I was assisted to the recovery room. There, I rested for a half hour, loopy from medicine and drinking my ginger ale, before I was released to my loved ones. While the process was both mentally and physically draining, I cannot praise enough the staff who provide these services for women in need.
It’s taken my husband and I some time to feel comfortable sharing our experience. We have a wonderful support system and are confident in the decision we made. That being said, our choice was, and remains, controversial. But it shouldn’t be.
In 2019, 629,898 legal induced abortions were reported to Centers for Disease Control and Prevention. The fact that we are trying to conceive and chose to have an abortion comes as a shock to many, but upon hearing our full experience, they begin to understand the gray area in an issue previously seen as black and white.
And while my hope is that sharing our experience will help to change perceptions, no pregnant person should have to justify their decision. The world should not play judge and jury to such an intimate and personal experience.
As fate would have it, I’m writing this mere hours after learning I am pregnant again. After two unsuccessful pregnancies, those two lines on the pregnancy test bring both trepidation and joy. The excitement of the possibility of growing our family cannot completely overpower the worry and fear of “what if.”
What if I miscarry? What if there are medical issues? These are rational concerns, but ones that cannot be answered; Only time will tell. What I should not have to worry about is not having the right to make the decision that is best for myself and my family, should complications arise. I should not have to worry about losing autonomy over my body. I should not have to worry about losing my voice. I should not have to worry about losing my choice. No pregnant person should.
Do you have a compelling personal story you’d like to see published on HuffPost? Find out what we’re looking for here and send us a pitch.